(Reuters)
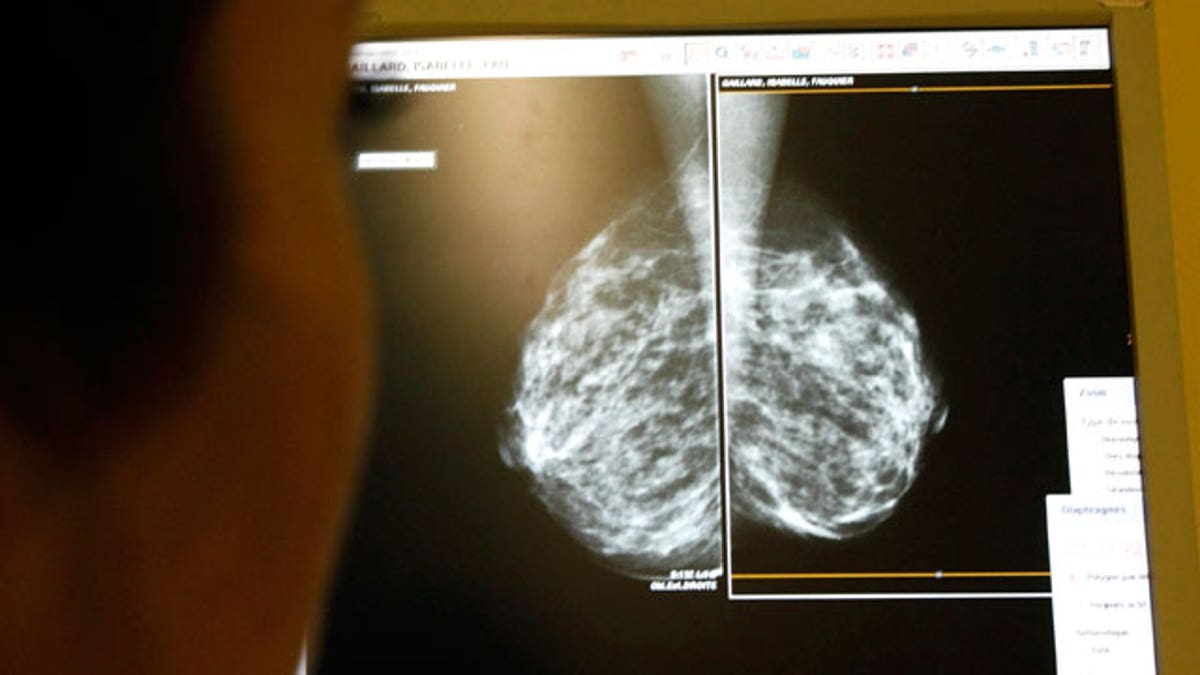
Women who are infected with a virus called the bovine leukemia virus (BLV) may face an increased risk of breast cancer, according to a recent study.
In the study, researchers tested the breast tissue of about 240 women for BLV, and found that 59 percent of the samples from women who had breast cancer showed signs of BLV. Only 29 percent of the samples from women without breast cancer showed signs of the virus.
The researchers' analysis of the data revealed that the odds of having breast cancer, when taking other risk factors into account, were three times higher if BLV was present — an increase that's higher than those of several other well known risk factors for breast cancer, including drinking alcohol, being obese and using hormone treatments after menopause, the study said.
BLV is frequently found in cattle herds throughout the United States, infecting the animals' blood cells and mammary tissues. Most cows do not become sick from the virus, although a very small percentage do develop cancer of the lymph system. [6 Things Women Can Do to Lower Breast Cancer Risk]
Researchers are still working to determine how the virus is transmitted to people. It's possible that dairy products and beef may be a source of infection, the researchers said. The new study did not determine how BLV infected the breast tissue samples.
"The most important thing now is to learn how humans get the virus," said Gertrude Buehring, the lead author of the new study and a professor of virology at the University of California, Berkeley's School of Public Health. "Is it coming from cattle, or is it coming from other humans?"
Researchers do know that in cows, the virus can quickly spread through a herd, because calves are sometimes fed from tanks that contain milk from several cows. When milk from one infected cow is mixed in with other milk, any calves that feed from that same pool, can become infected — even if their own mother is BLV-negative, Buehring said.
In a 2007 U.S. Department of Agriculture survey, researchers tested more than 500 U.S. dairy farms' "bulk tanks," which contain milk from many cows mixed together. The testing showed that milk tested positive for BLV antibodies at 100 percent of the dairy operations with large herds, of 500 or more cows. Even at small dairy operations, those with fewer than 100 cows, the milk tested positive for BLV in 83 percent of the operations, according to the survey.
Last year, Buehring led another study, published in the journal Emerging Infectious Diseases, that overturned the long-held belief that BLV could not be transmitted to humans. That research suggested the virus could be passed to humans through the consumption of undercooked meat or unpasteurized milk.
Yet the new study did not follow patients forward over time. So although it shows an association, it cannot determine whether there is a cause-and-effect relationship between the virus and breast cancer. However, Buehring noted, if future research does reveal that BLV can cause breast cancer, it could point toward a way to prevent cancer — potentially in the form of a vaccine against BLV.
Several vaccines have been created to protect people against viruses known to cause cancer. These include the hepatitis B virus, which can cause liver cancer, and the human papillomavirus (HPV), which can cause cervical and anal cancers. However, Buehring cautioned that making such vaccines isn't always possible.
"If it's caused by a virus, a vaccine may be a possible prevention method," Buehring said. Some researchers would like to shift the emphasis of breast cancer research to focus more on preventing the disease, she said. "But vaccines aren't always possible to develop, because every virus is different."
For now, researchers say they are still uncertain whether BLV may cause breast cancer. Dr. Michael Greger, director of public health and animal agriculture at the Humane Society of the United States and Humane Society International, who was not involved in the study, said it's also possible that cancerous breast tissue baits, or attracts, the virus. Greger, who is also a general practitioner specializing in clinical nutrition, has researched the public health implications of industrialized animal agriculture.
"Maybe there's something about cancerous breast tissue that somehow attracts the virus, or makes a good home for the virus," Greger told Live Science.
"The next step would be to follow women who have been exposed [to BLV], and individuals who haven't been exposed, based on antibody tests, and just see if women with exposure have a higher likelihood of going on to develop breast cancer," he said.
The study was published Sept. 15 in the journal PLOS ONE.
Copyright 2015 LiveScience, a Purch company. All rights reserved. This material may not be published, broadcast, rewritten or redistributed.







































