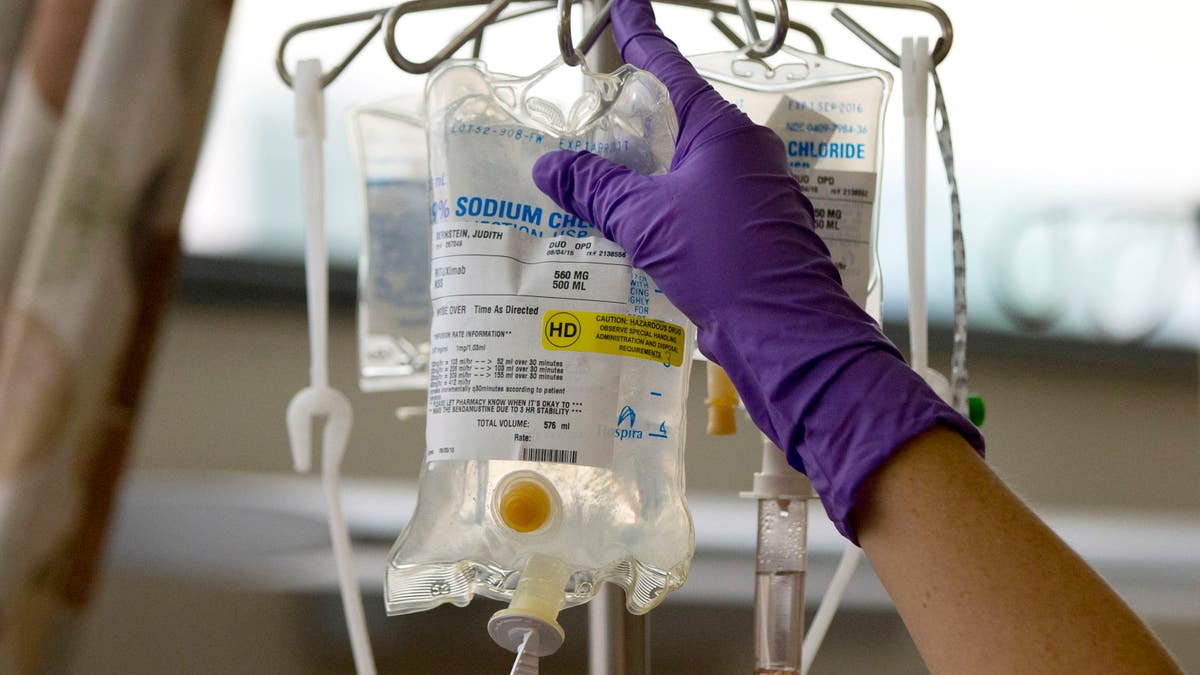
FILE - In this Tuesday, Aug. 4, 2015 file photo, a nurse places a patient's chemotherapy medication on an intravenous stand at a hospital in Philadelphia. A report released on Thursday, Jan. 7, 2016 says cancer is the second leading cause of death nationally, after heart disease. Cancer death rates have been falling for nearly 25 years, but heart disease death rates have been falling at a steeper rate. (AP Photo/Matt Rourke, File) (AP)
The National Cancer Moonshot – President Obama’s bold program to eliminate cancer as we know it – borrows part of its name from President Kennedy’s similarly audacious pledge to win the space race of the 1960’s.
Only this time, the stakes are even higher.
Announced in January, and jump-started with $1 billion in federal funding, Moonshot is intended – in the President’s words – “to harness the spirit of American innovation to identify new ways to prevent, diagnose, and treat cancer,” which kills about 1,500 Americans every day.
Since the announcement, a National Cancer Institute Blue Ribbon panel has been formed to prioritize the use of Moonshot funds. Seven working groups have been formed, which focus on specific research priorities. Plus, Vice President Biden will lend his passionate spirit to the leadership of Moonshot, inspired by the tragic loss of his son to cancer last year.
Moonshot is good. Very good indeed.
But I believe one of its key pillars is not receiving enough priority. And that is … early detection of cancer, before it spreads.
I think our very best opportunity in cancer medicine today is to figure out how to detect cancer earlier, leading to more cures for patients with limited disease and fewer patients having metastatic disease.
And that opportunity is to enhance cancer screening.
More Screenings; Less “Looks”
Don’t get me wrong. I am totally committed to cancer research, and have been for 30+ years. Without question, cancer research funding leads to knowledge that down the road will lead to better cancer treatments.
But every day, I walk through the lobby of our Cancer Center and see scores of cancer patients. I say hello, and sometimes we chat. Most of these people are here because they have advanced disease. Many know that their days are numbered. Invariably, patients tell me how grateful they are for our care.
But there is always that “look” in their eyes. It’s a look that says that cancer is terrible, that they do not want to die, that they are scared, that they are living a new normal that is unlike any “normal” they ever thought about.
And I wonder how many of them would not be there – and would not have that foreboding look – if more aggressive, equitable and technologically advanced screening practices had been in place for them.
Cancer screening detects cancer at an earlier stage, which allows more patients to be cured. In 2016, there will be 246,000 new cases of breast cancer in the US, and 40,000 deaths. But cancer screening reduces breast cancer mortality by 20%.
Also, there will be 135,000 new cases of colo-rectal cancer, and 50,000 deaths. But colo-rectal cancer screening reduces mortality by 33%. The results are even better for cervical cancer screening, which would reduce the current 4,100 annual deaths by well over 60%.
Unfortunately, not everyone who is an appropriate candidate for cancer screening gets screened. Overall, appropriate screening rates in the US for breast cancer (72%), cervical cancer (81%), and colo-rectal cancer (58%) leave thousands of people unscreened. If you are near or below the federal poverty threshold, screening rates drop significantly. —colo-rectal cancer screening drops to 44%. And if uninsured, the rates are even worse---falling to as low as 23% for colo-rectal cancer screening.
Proactive Programs Save Lives, Dollars
The cost to our healthcare system of these gaps in screenings is huge. By 2020, the direct and indirect costs1 of cancer in the US alone are projected to increase by as much as 39% to over $172 billion annually. Early screening and detection can help reduce that cost by catching the cancer before it has metastasized and a patient must endure costly cancer care.
A great example of how these screening gaps can be addressed is through a patient navigator program developed by Dr. Harold Freeman in 1990. The program is aimed at eliminating barriers to timely cancer screening, diagnosis, treatment, and supportive care. It has showed extremely promising results. It showed that navigators could dramatically increase the use of screening mammography, which improved five-year breast cancer survival rates at Harlem Hospital from 39% to 70%.
The issue of cancer care for the uninsured goes beyond screening. Data from the American Cancer Society shows that survival for patients with stage 2 colorectal cancer, who are privately insured, is superior to stage 1 colo-rectal cancer patients who are uninsured. This is appalling.
Navigation programs, new models of care in locations with high cancer mortality rates and patient-centered medical homes can successfully address such disparities in care and outcomes. They can do so today if resources were directed to such proactive programs. Tens of thousands of lives are at risk annually in the United States.
Let’s use Moonshot dollars to research this. Let’s fund pilot projects and demonstration projects with a goal of having all patients receive appropriate cancer screening, regardless of insurance or income status. If we do that, then fewer patients will show up in cancer centers needing newer targeted therapies to treat advanced disease in the first place.
The programs being funded by Moonshot are all worthy ones. But if we want to relieve suffering from cancer today, let’s put more effort – and funding – towards initiatives that are simple, proven and achieve results.
Let’s use a huge chunk of Moonshot resources to tackle this fundamental issue. Let’s help tens of thousands of people today.








































