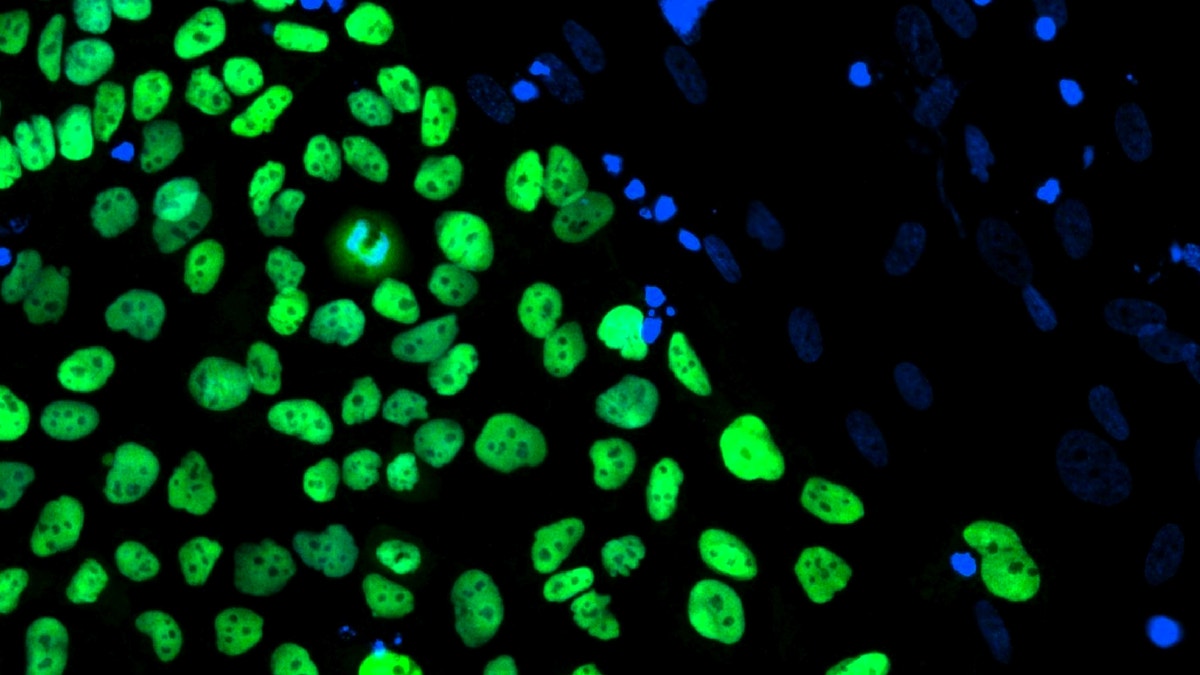
A human embryonic stem cell line derived at Stanford University. (REUTERS/Julie Baker/Stanford University School of Medicine/California Institute for Regenerative Medicine/Handout)
Type 2 diabetes is marked by insulin resistance, or the body’s inability to store sugar and convert it into carbohydrates for energy. Overcoming that resistance is the main hurdle scientists face in creating new treatment for the condition, but researchers in Canada have found a promising means for doing so: combining stem cell therapy and antidiabetic medication.
Type 2 diabetes accounts for nearly 95 percent of the 400 million diabetes cases worldwide. Current treatment often involves imprecise insulin injection, and can produce side effects like unwanted weight gain, gastrointestinal issues and low blood glucose levels. Eighty percent of Type 2 diabetes patients are overweight.
In the study, published Thursday in the journal Stem Cell Reports, scientists observed that transplanting pancreatic stem cells derived from human cells into mice with Type 2 diabetes symptoms, then administering common antidiabetic drugs, improved the mice’s glucose metabolism, body weight and insulin sensitivity— three hallmark problems associated with the condition.
“There have been similar reports looking at treatment of type 1 diabetes by stem cell-based replacement, and there are many people around the world who are interested in that,” lead study author Timothy J. Kieffer, a molecular and cellular medicine professor at the University of British Columbia, in Vancouver, told FoxNews.com. “Until this point, nobody to our knowledge had tested such a stem cell-based transplant study in a Type 2 diabetes model.”
Many people have predicted this approach to fail because one of the characteristics of Type 2 diabetes is insulin resistance and so it was generally thought that simply replacing insulin wouldn't be effective, Kieffer added.
Researchers fed four separate groups of immunosuppressed mice a different diet to try to emulate humans diagnosed with Type 2 diabetes. One group of mice received a 45 percent fat diet; one a 60 percent fat diet; one a high-fat, Western diet; and the last a low-fat diet. No single group of mice developed a phenotype that exactly mimicked a Type 2 diabetes human patient, but all three high-fat groups ended up exhibiting characteristics that mirrored the hallmark features of the condition.
Study authors transplanted human embryonic stem cell (hESC)-derived pancreatic progenitor cells into the mice after they began exhibiting symptoms. These cells are programmed to expand and differentiate when transplanted and to subsequently secrete insulin.
To transplant the human cells, researchers used a macroencapsulation device, a mechanism that is meant to prevent the body from detecting nonnative material as foreign and subsequently rejecting it. Because the mice were immunosuppressed, the device wasn’t necessary, but Kieffer said his team used it so their findings would be more relevant for future clinical trials, wherein the patients would not be immunosuppressed. Researchers opted to induce Type 2 diabetes symptoms in immunosuppressed mice with diet instead of using a mouse model genetically engineered to assume Type 2 diabetes for that same reason.
“The hope in the field is that some sort of device will eliminate the need for immunosuppression when cells are transplanted,” Kieffer said.
Twenty-four weeks after transplanting the cells into the mice, researchers saw only slight improvements in the animals’ Type 2 diabetes symptoms.
“Their ability to clear the glucose tolerance test was improved but not normalized— it was not comparable to the animals on the low-fat diet,” Kieffer said.
But after adding a low dose of one of three antidiabetic drugs to the mice’s food or drinking water, in 12 weeks, researchers saw dramatic improvements in their glucose tolerance. The drugs used in the study were sitagliptin, metformin and rosiglitazone.
“The drugs were ineffective on their own,” Kieffer said. “We had a group of animals that had drugs plus the cells. But we also had a group that only got the drugs and we didn’t transplant any cells— in that cohort of animals, the drugs were not effective at reducing body weight, improving insulin sensitivity and lowering glucose levels.”
“What was really surprising and unpredicted was that the animals [receiving the cells] lost a lot of weight, which wasn’t intended but was a very nice observation,” Kieffer added.
Kieffer said the human stem cells and the drugs appeared to work as a team, and that the cells appeared to help reduce the demand of the insulin. He said other animal studies are underway to test higher doses of cells for transplantation, as well as studies involving more mature pancreatic insulin-producing cells derived from hESCs on their own— without the use of antidiabetic medication.
“We’re hopeful that the therapy would work without any drug,” Kieffer said.
Similar research involving type 1 diabetes offers promise. A study published in the September 2014 issue of the journal Nature Biotechnology, which Kieffer helped author, indicated that mature pancreatic insulin-producing cells derived from hESCs, the same stem cells used in the current study, helped reverse type 1 diabetes. And a similar human stem cell-based transplantation method, using a macroencapsulation device, is currently underway in a clinical trial for type 1 diabetes patients. San Diego, Calif.-based company ViaCyte Inc. is conducting that study, which began in mid-2014, according to their website.
“I think it’s very exciting that both the FDA (Food and Drug Administration) and now [Health] Canada have reviewed the studies ViaCyte has done and cleared them to go to clinical trial,” Kieffer said. “I think that really paves the way for other sorts of studies in this field, such as ours.”







































