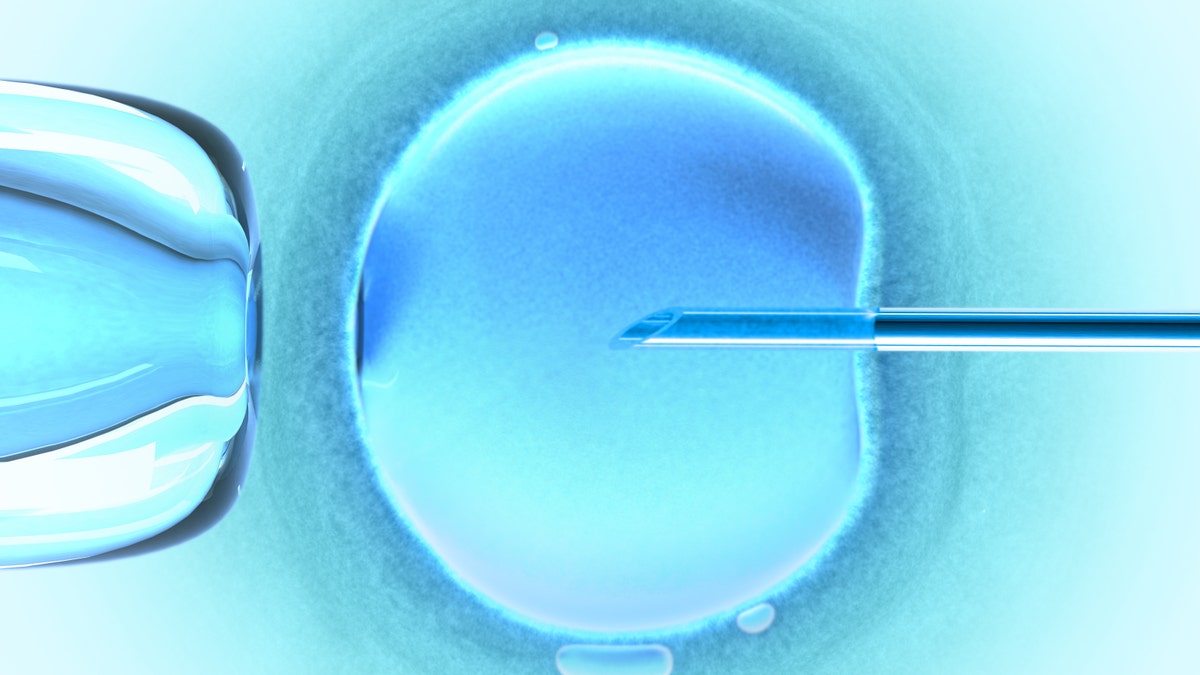
(iStock)
When undergoing IVF, you're hormonal from all of the drugs you take, you're bloated from the doctor stimulating multiple follicles at once, and—if all goes according to plan (though it sometimes doesn’t)—a human embryo is put into your body. At this point, the doctor tells you not to drink alcohol or overly exert yourself because you may be pregnant. It's a real mind trip when you've been trying to conceive unsuccessfully for months or in many cases, for years...
IVF isn't for someone who is scared of needles or who doesn't have time to hang out at the doctor's office every 24-72 hours for weeks on end. It's also not for someone who isn't prepared to spend thousands and thousands of dollars on something that may or may not work.
Going through infertility and fertility treatments hits us on every level: emotionally, physically, financially, and even spiritually. This stressful process also rocks our relationships; it can also be very isolating to go through infertility, as most people don't openly discuss their experience. That's why I founded pregnantish—and why I was thrilled when Anna Beard agreed to share her experience with me so I could share it with the readers of Prevention. —Andrea
Anna's story
I've been TTC (trying to conceive) with my husband of five years since June 2015, when I was 34. Even though I suspected I'd have an issue due to spotty periods and strange cycles, I didn't visit a fertility specialist until October of 2015. Initially, I didn't think I'd try IVF: I'd heard it was a nightmare, plus I figured I'd just need some minor intervention and be on my way to a healthy pregnancy.
AUTISTIC TEEN DELIVERS CRAYONS, COLORING BOOKS TO SICK CHILDREN
That's not what happened. In January 2017, after a couple of years of trying naturally, having many tests and procedures, and experiencing multiple failed IUI (intrauterine insemination) treatments, my husband and I finally decided to do IVF.
At the end of February, a week before my period was due, I headed to the fertility clinic to start prepping my body for the procedure.
The week before my period starts
I never thought I would need IVF and am nervous to start, but after so many failed IUI cycles, it's time. This whole thing is draining already.
I'm at Johns Hopkins Fertility Center at Green Spring Station in Timonium, Md. It's a teaching hospital, so it's normal to be seen by residents and students. I'm okay with this, as we're learning about it, too.
My husband and I are told that before starting IVF, we need to get all kinds of authorizations done through our clinic's Financial Coordinator and through our insurance company. We are also instructed by the nurse to get all medications ordered. It is a lot of medication. (Apparently you get everything you need up front because based on your blood work you won't really know what you have to take until day of.)
Being on the phone this week with the insurance company is stressful and time-consuming. It's a hassle to get all of the authorizations, and I'm worried we won't get the medication on time to start this IVF cycle.
Ugh. I'm stressed and haven't even started the medications and injections yet... I end up having to borrow some medication from my doctor's office so it won't mess up my timing.
Meanwhile, my husband has to get another semen analysis. (It has to be within 6 months, so even though he's done it before for our IUI procedures, he needs to repeat it now). And we both have to do blood testing for HIV, hepatitis, syphilis, etc.
Week 1
On Day 2 of my menstrual cycle, I go in for the blood work and an ultrasound. Yes, during my period. This part of the process makes me so uncomfortable, but I'm grateful it's quick and that they made sure I didn't see any of the "mess."
My husband and I have to sign a bunch of consent forms at the clinic. More paperwork! We have to decide things like what we want done with any leftover embryos, since our clinic is part of a research hospital. This is a hard decision and my husband and I can't agree. We have a difficult argument and decide to stop talking about it for now.
CHARLIE GARD CONTROVERSY: WHAT CAUSES INFANT'S RARE CONDITION?
The injections start right after my blood test results. I didn't expect this and have a hard time with these shots—many times I either spill some meds or use the wrong needle to mix—even though we previously attended an IVF class that taught us about all the different injections and needles and how to mix medication.
I'm freaking out and worrying that I'm doing it all wrong.
After being on drugs for a few days, I go back to the clinic for blood work and an ultrasound and am told that I have 21 follicles and really high estrogen. (Most women have two ovaries and each ovary contains follicles, sacs that each have an egg in them. At the start of IVF, the ovaries are in the "resting" stage, and after a few days of medication they start growing in quantity and size.)
The doctor instructs me to cut my injections to half doses. I guess everything is growing fast.
On Day 6, I go for another ultrasound.
Week 2
I'm starting to go for regular blood work and ultrasounds at the clinic. They have to track everything to see how I'm responding to the medication and how my follicles are growing.
I'm really lucky I have a flexible work schedule because I work for myself. I cannot imagine how someone who needs to go to an office every day can go through IVF.
On Day 8, they tell me that I have 25 follicles. I'm told some follicles are on track and above 13mm. This is a good thing—follicles need to be approximately 15-23 mm before a doctor can retrieve them—but I have a swollen belly and am totally uncomfortable.
I return for another ultrasound and more blood work on Day 9, the next day, and I'm instructed to take a shot that night to stimulate ovulation. The trigger shot releases the eggs 36 hours later.
On Day 11, I'm back at the clinic and put under anesthesia for my egg retrieval. They retrieve 25 eggs. This is good, but I'm groggy and feel so uncomfortable.
On the bright side, part one of IVF is done! Now that they've retrieved my eggs, they're going to try to fertilize them with my husband's sperm. I should be relieved, but I feel yucky.
The next day I'm on the toilet almost all day. I have prune juice because I'm so backed up and have extreme belly bloat. I drink a ton of Gatorade because that's what they told me to do, but I wish I had stuck with Pedialyte or coconut water because the Gatorade has so much sugar and makes me feel even more sick.
The clinic calls during this time and says that eight eggs fertilized. I'm bummed by this number; I thought it would be higher since we started with 25 eggs, but they seem happy with the result.
Over the next few days I gain five pounds and feel terrible.
Week 3
I start new medication, which includes a steroid, an antibiotic, and estrogen pills. I'm also instructed to start progesterone gel suppositories twice a day. They are preparing my body for implantation and trying to prevent infections.
Three days after my egg retrieval, the clinic calls to give me the cell count and grade for each of the 8 eggs that fertilized into embryos. The goal is to assess cellular development and move these embryos to blastocyst stage (a more complex embryo structure made up of about 200 cells) on Day 5.
CANCER VACCINES HELP PATIENTS GET TUMOR-FREE IN 2 STUDIES
My numbers don't seem that great, but the nurse reassures me that she's seen healthy babies come from average embryos and that they could improve by day 5 in the petri-dish.
Five days after my retrieval, I go back into the clinic for my "fresh" embryo transfer. (This is the point when they put the embryo that has been growing in the lab into your body.) By now, I'm feeling much better.
An hour before the transfer, I have to drink a full large bottle of water, because they need to insert the embryo with a full bladder so they can see better and have better placement. I'm so uncomfortable, and I learn that a different doctor is on duty. I'm upset because I wish my own doctor was here to do the transfer.
I thought this procedure would be like an IUI, but it was a bit painful for me because they go higher up to place the embryo in the right spot. Good thing my husband was in there so I could squeeze his hand off!
The doctor transfers one "excellent quality and high grade" embryo and tells me they'll freeze the other four embryos.
They give us a printout of the embryo they put in my body and I'm feeling hopeful.
Week 4
I'm staying occupied but also taking it easy this week because I may be pregnant. I keep looking at the printout of the embryo that the clinic gave us. Our little embryo is adorable! I'm feeling excited that this may finally lead us to our baby.
I have some lower belly bloat this week and feel crampy. I've heard this can be symptom of late implantation and this excites me, but I'm trying not to obsess over every little thing. (In the past, I've spent way too much time on TTC forums reading into everything!)
I'm pretty confident that this is it. After two years, it's finally worked. The doctor said we had a "beautiful embryo" and I'm feeling pretty relaxed and strangely enjoying the wait to find out for sure.
Oh! And my breasts are enlarged and sore, I have lower back pain, and my skin is glowing. This feels like pregnancy stuff!
My husband's not usually the nurturing type, but he's being really helpful this week. He knows I had a tough time with the retrieval and realizes I could be pregnant, and he's being very caring. (He'll be a good dad!)
I haven't talked to my husband about my symptoms or the fact that I think this has worked, because I kind of want it to be a surprise (though with IVF, this old-fashioned notion of surprising your partner kind of goes out the window since everything is tracked).
We get our results soon, 10 days after the embryo was transferred into my body. I'm feeling relaxed and hopeful.
Am I pregnant?
It's 10 days later and the IVF nurse left a voicemail to say that the beta blood test was negative. I'm totally shocked as I was sure it worked. She sounds upset. I don't want to accept this. Maybe I have late implantation. I mean, I wouldn't feel all of these symptoms, right?
I start reading all the forums again and I see that maybe it's negative because of late implantation, so I still have a glimmer of hope. I'm also trying to come to terms with the fact that it may actually be a failed cycle and I'm totally devastated.
I'm really anxious to find out why this hasn't worked. Is it genetics? Hormones? Adrenal? Have I been too stressed and is that affecting my hormones?
I email the doctor because my mind is spinning. He calls me back (which surprises me as we never talk on the phone), and he admits that he's also disappointed that it didn't work as the whole team there really thought it would. It was a beautiful embryo.
He suggests we move forward with genetic testing for the other embryos we have frozen, to ensure that they're healthy. It's an additional cost, but it seems like a good idea.
Right now I don't want to do anything but curl into a ball in the corner....
Today (June 2017)
We decided to have the embryos genetically tested and then take a few months off, so the period from March to June has been uneventful and enjoyable. I didn't have to worry about ultrasounds, blood work, injections, medication, eating well, drinking enough water, taking my vitamins, and whether I was getting too much activity. All the stress just vanished.
Thanks to all the medication and fear of over-exercising, I put on about 10 pounds in the last year. But since my failed IVF attempt I started doing short workouts every day and I'm feeling great. And I'm hoping to continue working out and not putting pressure on myself to be the perfect IVF patient because I felt like I was losing myself. We have lots of stuff coming up to prepare my body for a frozen embryo transfer in July.
Hoping for the best.
This article first appeared on Prevention.
