
Amid an epidemic of addiction and abuse tied to these powerful opioids drugs, the CDC is urging general doctors to try physical therapy, exercise and over-the-counter pain medications before turning to painkillers for chronic pain. (AP Photo/Toby Talbot)
Florida’s largest health insurance company will stop covering one of the most widely used -- and abused -- prescription opioids amid a nationwide drug abuse epidemic.
Florida Blue said Monday that starting Jan. 1, 2018, it will no longer cover the cost of OxyContin, or oxycodone, prescriptions and instead offer patients Xtampza ER. That drug turns into a gel when crushed, so it cannot be easily snorted or smoked. Further, when Xtampza is crushed it releases a substance, known as an opioid antagonist, that minimizes the effect of the opioid.
“Most physicians, most plans have had a hands-off approach for a number of years, and we see where we are now,” Scott McClelland, Florida Blue’s vice president of commercial and specialty pharmacy, told the Miami Herald. “We think it’s time for more people, including physicians in our community, the nurses, even the families to take a more proactive approach in trying to manage this epidemic.”
McClelland added that the switch is part of a new approach Florida Blue is taking to combat the rising abuse of opioids in the country. In May, Florida Gov. Rick Scott announced a statewide public emergency and, more recently, federal officials declared a national opioid overdose epidemic.
“The individuals struggling with drug use are sons, daughters, mothers, fathers, sisters, brothers and friends and each tragic case leaves loved ones searching for answers and praying for help,” Scott said. “Families across our nation are fighting the opioid epidemic and Florida is going to do everything possible to help our communities.”
Nationally, more than 52,000 Americans died from drug overdoses in 2015 and that number has been rising drastically in recent years. More than half those deaths involve prescription opioids.
In Florida, opioids killed 2,538 people in 2015 and contributed to the deaths of 1,358 other people.
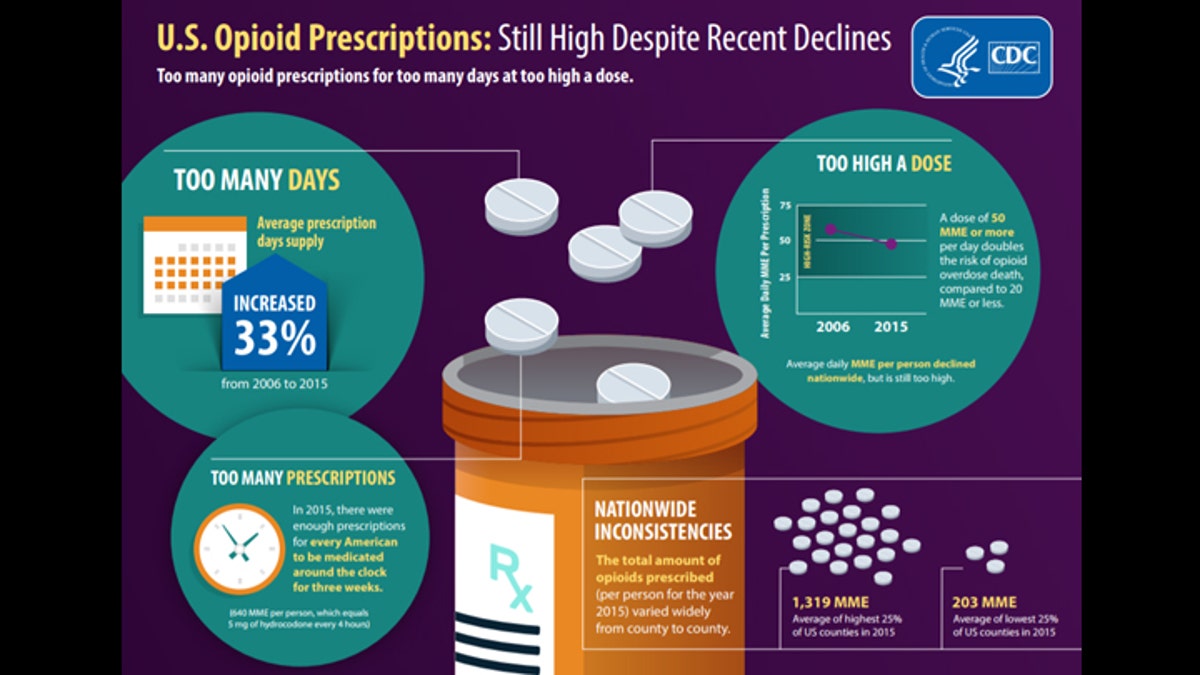
(CDC)
McClelland thinks that prescribing Xtampza ER instead of OxyContin will not only curtail the rampant number of overdose deaths, but also have an effect on street prices.
“It makes the street value a lot less because it’s harder to manipulate,” McClelland said.
Florida Blue’s latest move follows in the footsteps of its 2015 policy that requires prior authorization for all oxycodone prescriptions of more than seven days. That policy, the company says, led to a 20 percent reduction in the use of long-term opioids by members over 12 months.

medical bottle and pills on background (DimaSobko)
Other insurance companies have also taken steps to replace OxyContin prescriptions with Xtampza ER, with Cigna announcing in October that it would stop covering the former.
While Purdue Pharma, which manufactures OxyContin, says it supports limiting the supply of the drug, the company added that Florida Blue’s policy will make it tougher for doctors to address addiction among their patients and that Xtampza ER comes with its own potential for abuse.
“Florida Blue’s decision limits prescribers’ options to help address the opioid crisis,” Danielle Lewis, a Purdue Pharma spokeswoman, said in an email to the Herald. “Further, while both products are formulated with properties designed to deter intranasal [snorting] and intravenous [injection] abuse, neither is abuse proof.”







































