DR. MANNY: Another tragedy demands greater outpatient transparency
{{#rendered}} {{/rendered}}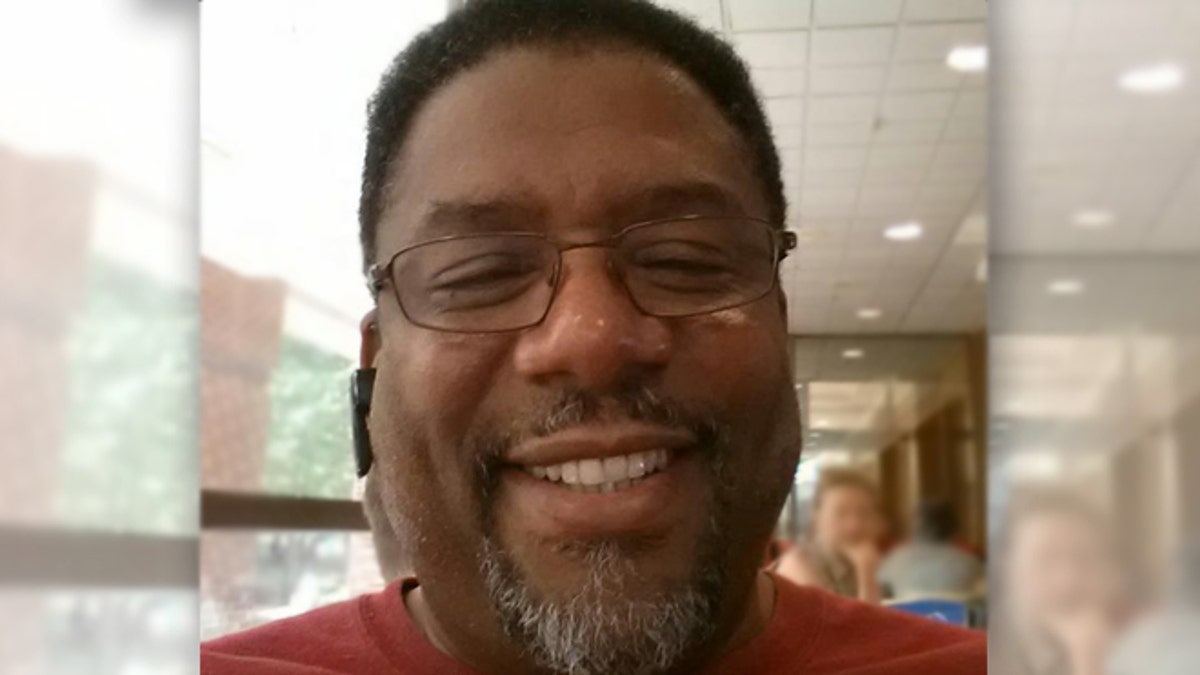
Michael A. Palmer, a 58-year-old father of eight died in May 2013 during a cervical spine fusion procedure at an outpatient clinic in Connecticut. (Facebook)
The family of a Connecticut man who died during an outpatient procedure is suing the center and the medical team for medical malpractice after doctors allegedly convinced the man to have the operation at an outpatient clinic where they were part owners, FoxCT.com reported.
Michael A. Palmer Sr., a 53-year-old father of eight, was undergoing a cervical spine fusion procedure when he died in May 2013. The suit alleges that Palmer’s medical team attempted an unauthorized procedure and administered a lethal dose of medication, according to FoxCT.com. Palmer had reportedly asked that the surgery be performed at a hospital, but members of his medical team had instead persuaded him to have it done at the outpatient clinic where they had vested financial interest, called Surgical Care Affiliates, LLC, which operates 185 surgical centers nationwide and the Surgery Center of Fairfield County.
This story is eerily reminiscent of the tragic death of comedienne Joan Rivers in September of last year. Rivers’ death was the first time a national spotlight was cast on the safety of these outpatient surgical clinics and whether or not they are equipped to handle medical emergencies that can arise on the operating table.
{{#rendered}} {{/rendered}}Now, this is not to say that all outpatient surgical facilities are not quality care centers. There are many of them which have popped up around the country to provide cost-effective ambulatory services on an outpatient basis and good clinical outcomes at affordable prices. However, it is also true that due to the terrible health care environment physicians and patients are currently dealing with, ethical lines are being crossed and proper monitoring of these centers sometimes falls short.
I have always worked in hospitals. Most of the colleagues I work with also work in hospitals and do so because in a hospital you have systems of checks and balances; you have protocols created to enforce patient safety, physicians are constantly monitored and credentialed after proper training and there are no conflicts of interest, as this case alleges.
It’s scary to think that in some outpatient clinics now you have vested interest placed in the hands of surgeons who, for one reason or another, choose to perform a procedure knowing full well that that center may be ill-equipped to handle an emergency.
{{#rendered}} {{/rendered}}For-profit chains of surgical centers need to be better regulated. If you look at the details of the lawsuit, the family claims that there may have been some violations with regard to how Palmer was monitored throughout the surgery and especially with the types of medications used during the spinal fusion.
According to the suit, a surgical assistant allegedly pressed against a blood pressure cuff during Palmer’s surgery, causing a drop in blood pressure reading and prompting the anesthesiologist to negligently administer 4 percent Lidocaine, a toxic agent, mistaking it for the agent, Hespan, a drug used to increase plasma volume during shock caused by bleeding, burns, surgery or other trauma . Allegedly, the 4 percent Lidocaine medication had been stored in the wrong place.
When the anesthesiologist called a “code blue” in response to Palmer’s reaction to the medication, the suit continues, medical staff tried to revive Palmer with CPR, and he was rushed to a local hospital where he died.
{{#rendered}} {{/rendered}}The lawsuit also alleges that the defendants violated state regulations by allowing a kind of procedure to be performed that was not authorized by the center’s governing body.
Consumers need to be aware of the potential for these kinds of transgressions within the current health care environment when it comes to outpatient clinics that are not as heavily regulated as hospitals and medical centers. Unfortunately, many times patients do not ask questions, but it’s imperative that they do.
When it comes to providing safety records and a clinic’s ability to handle medical emergencies, there also needs to be more transparency and full disclosure before a patient goes in for surgery.
{{#rendered}} {{/rendered}}We learn in medicine to “First, do no harm.” At the end of the day, it’s not about dollars and cents. It’s about providing quality care and making sure that patients have the best outcomes possible -- because in surgery complications can happen at any minute -- and sometimes it’s a matter of life and death.
