Treating America’s Pain: Unintended Victims of the Opioid Crackdown, Part 2 – The Doctors
As federal and state agencies respond to the staggering rate of drug overdose deaths -- primarily involving illegal opioids like heroin and illicit fentanyl -- doctors who maintain they are responsibly prescribing opioids are getting caught up in the crackdown. This is their side of the story to the opioid crisis and how it has impacted -- and for some ruined -- their lives.
This is the second of a three-part series on the nation's struggle to address its crippling opioid crisis, and the unintended victims left in its wake. Read Part 1 here: As doctors taper or end opioid prescriptions, many patients driven to despair, suicide.
Dr. Stephen Nadeau received a warning from the Gainesville, Fla., hospital where he worked.
Their policy on prescribing opioids was changing, to go beyond federal guidelines aimed at the national overdose crisis that has claimed hundreds of thousands of lives.
The hospital would stop treating pain with opioids. And every doctor, including Nadeau, had to stop prescribing them. Doctors otherwise risked losing hospital admitting privileges – and perhaps even their medical license.
In Helena, Mont., Dr. Mark Ibsen was feeling heat from the state medical board – and the U.S. Drug Enforcement Administration (DEA), for the high-dose opioids he was prescribing to patients in severe, chronic pain. An allegation made by what he described as a disgruntled employee charged Ibsen was overprescribing.
As a result, the state medical board suspended his license. The DEA visited five times, Ibsen said, suggesting he was risking his livelihood and could end up in jail if he kept prescribing.
Both doctors complied and stopped prescribing, affecting roughly 230 of their patients. Tragically, among those were several who committed suicide, the doctors said, when they couldn’t find another health care provider to relieve the pain.
That’s a scenario playing out across the country, as government agencies respond to the staggering rate of drug overdose deaths, involving primarily illegal opioids like heroin and illicit fentanyl. Doctors who maintain they are responsibly prescribing opioids are getting caught up in the crackdown, according to dozens of medical care providers interviewed by Fox News, leaving little room to both play by the rules and properly treat huge numbers of patients who legitimately suffer chronic and intense pain.
Some doctors like Ibsen and Nadeau are opting to simply stop prescribing legal opioids, as insurers, pharmacies, and authorities warn them about overstepping guidelines issued in 2016 by the Centers for Disease Control and Prevention (CDC).
Meanwhile, other doctors, nurses and medical associations accuse the federal government of interfering in the physician-patient relationship, and pursuing simplistic, politically expedient solutions that put tens of millions of Americans at risk.
“Not only is the government legislating the way we care for chronic pain patients,” said Nadeau, a professor of neurology at the University of Florida College of Medicine, “they are substantially taking away our ability to do it.”
CDC GUIDELINES CONTROVERSY
Critics of the way the 2016 guidelines have been applied note they were not intended as law, but as a means to advise primary care physicians. The CDC specifically cautioned against abruptly stopping or forcibly tapering opioid treatment for patients already taking them, because of the danger of withdrawals, or debilitation.
More than 300 health care professionals, including former drug czars in the Clinton, Nixon and Obama administrations, have signed an as-yet unpublished public letter to the CDC, warning of a brewing crisis among pain patients, despite the “laudable goals” of the guidelines.
“Within a year of (CDC) Guideline publication, there was evidence of widespread misapplication of some of the Guideline recommendations,” said the letter, written by three doctors and a pharmacist. “Soon, clinicians prescribing higher doses, pharmacists dispensing them, and patients taking them came under suspicion.”
“Patients with chronic pain, who are stable and, arguably, benefiting from long-term opioids, face draconian and often rapid involuntary dose reductions,” the letter continued. “Often, alternative pain care options are not offered, not covered by insurers, or not accessible … Consequently, patients have endured not only unnecessary suffering, but some have turned to suicide or illicit substance use. Others have experienced preventable hospitalizations or medical deterioration.”
Others argue many authorities have misunderstood, or outright ignored, the CDC’s disclaimer. Health care providers who don’t drop opiate painkillers are setting strict limits on dosage limits, even for chronic pain sufferers who require more medicine because of serious conditions, or the way they hyper-metabolize opioids. Many who do so cite the CDC guidelines, saying they were told to follow them -- or took them up as a kind of pre-emptive strike.
Not only is the government legislating the way we care for chronic pain patients, they are substantially taking away our ability to do it.
Dozens of pain patients have told Fox News they were dropped or forcibly tapered down by doctors who long treated them quite successfully, but who became fearful about losing their license after being formally admonished, or hearing about other doctors who ran afoul of the government.
Meredith Lawrence, who lived in Tennessee with her husband, Jay, while he suffered decades of pain following a tractor-trailer accident, recalled the helplessness she felt watching him suffer, while his dosage of opioids was being sharply reduced.
Lawrence said the doctor who had treated him successfully for years was very clear about his decision to taper down the dosage.
“He said ‘My patients’ quality of life is not worth risking my practice or my license over,'" she told Fox News. "I’ll never forget that.”
“Jay felt like they gave up on him,” she said, recalling what finally prompted her husband to kill himself. “That was the day Jay gave up. He felt the doctor gave up – and he gave up.”
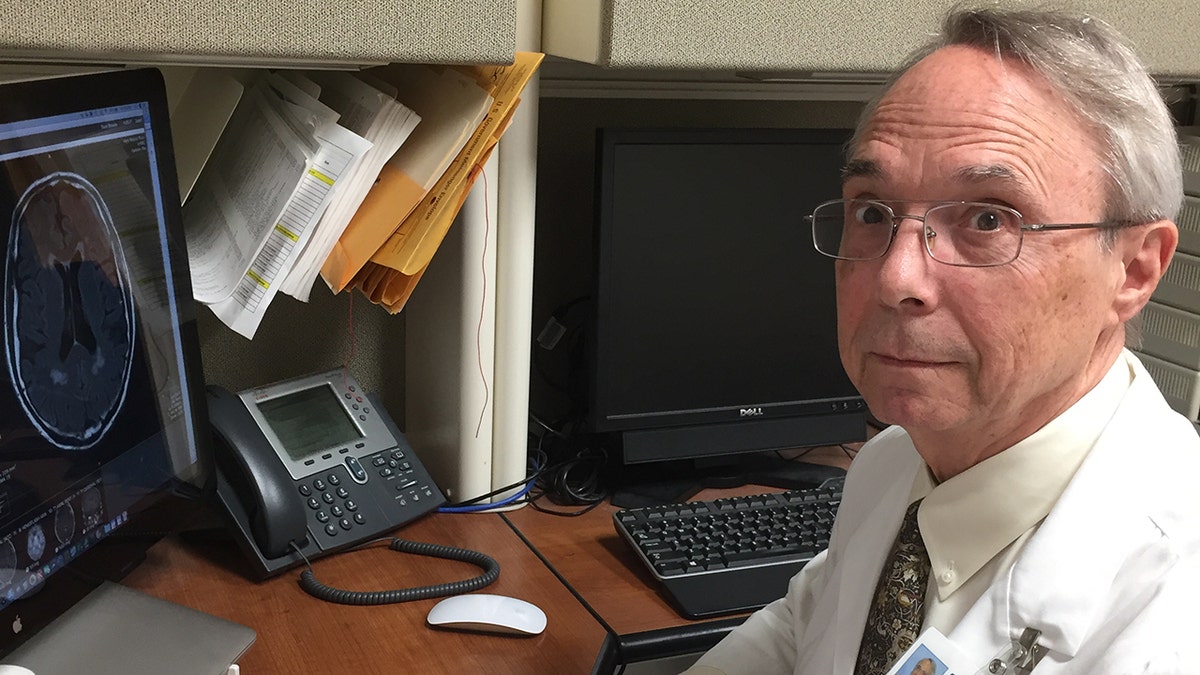
Dr. Stephen Nadeau
DEA TARGETING ‘WORST OF THE WORST’
Much of the opioid overdose epidemic in recent years stems from illegal drugs, not legitimate prescriptions. But more than a decade of overprescribing – out of ignorance for some, and for others the chance to rake in big profits – played a significant part, according to federal authorities and others who have studied the issue.
Assured by what some charged were deliberately deceptive pharmaceutical companies insisting opioids weren’t very addictive, some health care providers prescribed liberally, even for minor procedures such as a pulled tooth, or non-serious orthopedic injuries. Overprescribing led to greater daily dosages or easy-to-get refills – more than were needed. That, along with the theft and resale of opioids from people who had prescriptions, laid the groundwork for the crisis.
Most prescribers say they recognize many health providers were not prudent enough when prescribing opioids. And many doctors noted they were previously criticized for undertreating pain. Medical schools devoted little time to the study of pain and to opioids, they also say.
“Physicians and particularly medical school residency programs should have been taking more responsibility. Pain is the most common condition, and it’s one of the most difficult to treat,” said Nadeau. “And there [have been] pill mills that have relied on physicians to prescribe and many have done so very irresponsibly. But I think many are compassionate physicians ... it’s a reflection of the inadequacy of their training that they basically had to learn the ropes on their own.”
John Martin, the DEA’s Administrator of the Diversion Control Division, said an overwhelming percentage of prescribers followed the rules. Of 1.6 million registrants, he said, less than one percent “operate outside the law.”
But there are still unscrupulous prescribers.
“Remember, with the opioid epidemic, just one practitioner that’s operating outside the law can really have a lot of serious consequences. In a small community, it can wreak havoc,” Martin said. “They’re really going after the worst of the worst of the criminal violators.”
Martin said most prescribers have nothing to worry about.
“Doctors are writing less prescriptions. And that goes down to education with the CDC guidelines," he said. "There's a new and different way of looking at using opioids for chronic pain.”
But that’s not what prescribers and patients see.
“Doctors around the country are terrified because of what happened to me and other doctors,” Ibsen said. “We don’t arrest car dealers if someone drives a car and gets into a fatal accident.”
“Standards of care are being decided by a jury of people without medical training,” Ibsen added. “It’s a very bad situation. We’re playing Whack-a-mole with the wrong mallet.”
Remember, with the opioid epidemic, just one practitioner that’s operating outside the law can really have a lot of serious consequences. In a small community, it can wreak havoc...[the DEA agents] are really going after the worst of the worst of the criminal violators.
THE CHALLENGE OF PAIN MANAGEMENT
For many medical professionals, treating pain patients has become a thankless task. The stakes are too high, they say, as even those who try to responsibly manage opioid treatment for their sickest pain patients find themselves hounded by authorities or pharmacists.
Many doctors say they view opioids as a last resort. They are very strong medicines, which often come with strong side effects, ranging from constipation, nausea, liver damage and respiratory problems. Many pain patients said in interviews they were reluctant to take them initially, and eventually did only after other treatments and surgeries failed.
“If we had a good alternative to opioids, every physician would be at the front line of it to prescribe that,” said Dr. Lynn Webster, vice president of PRA Health Sciences, and the past president of the American Academy of Pain Medicine.
In a recent survey by the North Carolina Medical Board of its licensees, 43 percent of 2,661 respondents said they had stopped prescribing opioids. They attributed their decision to concern about getting into trouble.
Patients complained to the board doctors had cut them off, pointing to the CDC guidelines or an initiative by the board aimed at cracking down on health care providers who prescribed high doses of opioids, or who had two or more patients die of overdoses in a year.
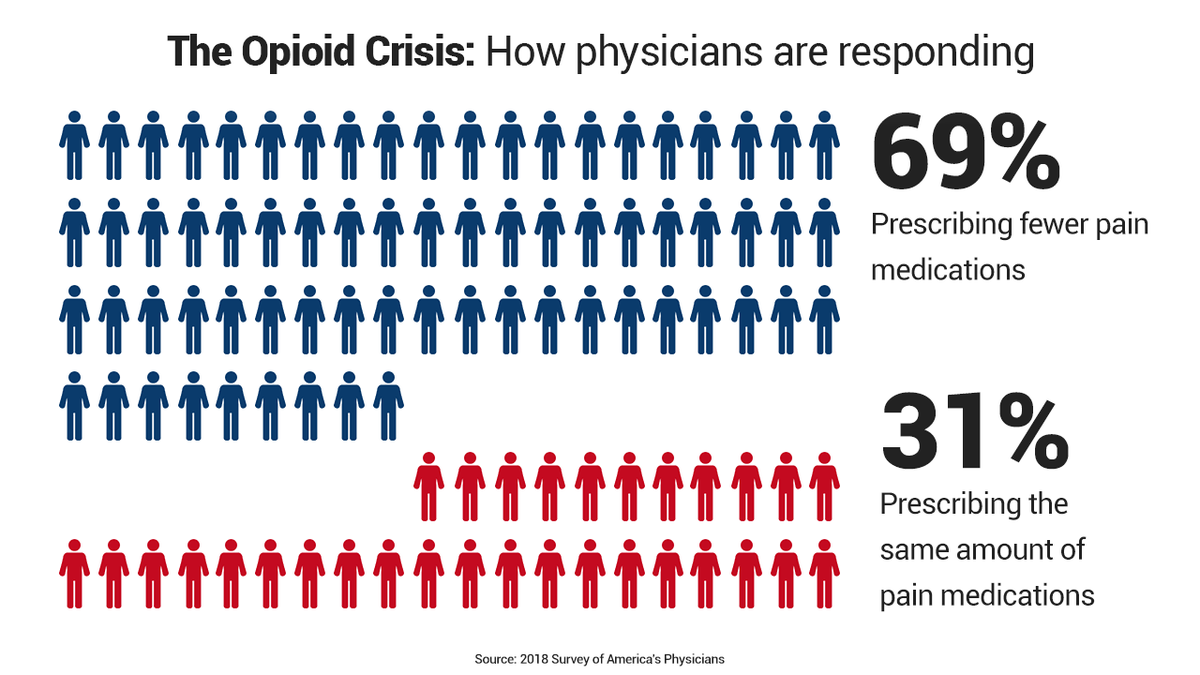
And of 3,000 doctors responding to a recent nationwide survey by the SERMO physician network for BuzzFeed News, 70 percent said they had dramatically cut down or altogether stopped prescribing opioids. The main reasons were “too many hassles and risks involved,” “improved understanding of the risks of opioids,” and fear of “getting into trouble,” according to BuzzFeed.
Yet another survey, commissioned by The Physicians Foundation, showed about 70 percent of nearly 9,000 physicians nationwide were prescribing fewer opioids.
In Nevada, where so many doctors stopped taking pain patients after the state implemented strict opioid prescription rules – which increased required record-keeping – physicians like Dan Laird now have a six-month waiting list.
“We turn patients away every day,” said Laird, who last year could fit in patients soon after they called for an appointment. “It’s heartbreaking, but many can’t find doctors.”
Many pain patients told Fox News that after being forcibly tapered down or abandoned by their pain doctors, they have lost much of their ability to function. Many said they have made suicide plans.
"I have heard from -- either through email or posts on my blogs -- about 1,000 people over past two years who have been denied pain medicine or forced to dramatically reduce their dose who have expressed a desire to die or commit suicide," Webster said.
Kate Nicholson, a former federal prosecutor who credits her opioid treatment with allowing her to function after years of being bedridden, said: “We’re looking only at the supply, and cutting off people who are not abusing the medication. It made all the difference in the world, I couldn’t sit or stand or walk because of nerve damage. I went from being bed-ridden and completely non-functional to doing my work as a prosecutor.”
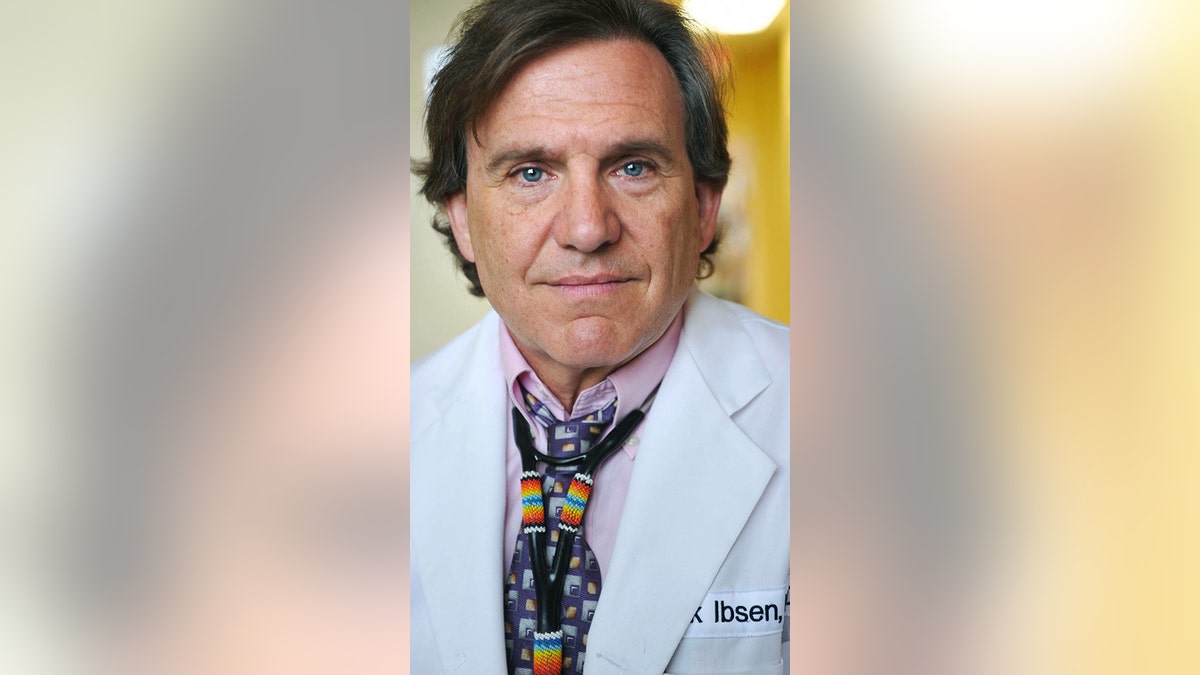
Dr. Mark Ibsen
WARNINGS, RAIDS AND ARRESTS
Health care providers who prescribe opioids, particularly to high-impact chronic pain patients, are finding themselves on the radar of any number of sources – pharmacists, state medical boards, insurers, and law enforcement.
In a speech about the national overdose deaths epidemic in March, President Trump said: “Whether you are a dealer or doctor or trafficker or a manufacturer, if you break the law and illegally peddle these deadly poisons, we will find you, we will arrest you, and we will hold you accountable.”
But the red line triggering disciplinary action often is inconsistent, and murky. The CDC considers an opioid’s benefits to outweigh risks if it improves pain and function by at least 30 percent. But, doctors say, those factors rarely are considered when authorities scrutinize prescribing patterns.
More often, it’s large amounts of opioids and high doses – statistics on a spreadsheet or chart, without the context of a patient’s medical condition -- that can bring disciplinary action.
On Nov. 2, Dr. J. Julian Grove posted to Twitter a letter his Phoenix office had received from Walgreens. Grove said he wanted to provide chronic pain patients “an insight to the veiled threats” that health care providers treating pain are getting these days.
The letter said: “Walgreens has determined that you may have issued prescriptions for opioids that exceed the CDC guidelines.”
It said Walgreens had the right to refuse to fill a prescription that falls outside the guidelines, and added: “Walgreens pharmacists may notify appropriate regulatory agencies when prescriptions are refused.”
Grove blasted the letter.
“I am a double board-certified anesthesiologist and pain specialist, treating complex pain and cancer pain always w/comprehensive approach," he said. "Insulting.”
Asked about Walgreen’s pressure on prescribers to follow the CDC guidelines, company spokesman Phil Caruso told Fox News in a statement: “As a key patient touchpoint in the nation’s healthcare delivery system, we regularly communicate with prescribers to help ensure the safe and effective dispensing of medications in the best interest of our customers ... Fighting the opioid epidemic requires all parties, including leaders in the community, physicians, pharmaceutical manufacturers, distributors, pharmacies, insurance companies, PBMs (pharmacy benefit managers) and regulators to play a role and coordinate efforts.”
The U.S. Attorney’s Office in Atlanta announced in October that some 30 doctors were put on notice there for prescribing opioids in larger quantities and higher doses than others. Prosecutors enclosed the CDC guidelines with the warning letters.
U.S. Attorney B. Jay Pak called those doctors “outliers,” adding the warning letters were meant to point out “atypical practices.” Significantly, Pak said the doctors may not have done anything wrong.
“It is our plan to strategically reduce the impact of this crisis within our community by notifying outlier prescribers that their opioid prescribing habits are not in conformity with accepted standards, or the prescribing habits of their peers,” the agency said in a statement. “Through this initiative and others, it is the goal of the Department of Justice to reduce opioid prescriptions by one-third over the next three years.”
Prescribers particularly dread getting in the crosshairs of the DEA, which can revoke permission to manufacture, distribute and dispense controlled substances. The agency opens about 1,500 new opioid cases per year and makes more than 2,000 arrests. The arrests include DEA registrants, doctor-shopping patients, and prescription forgery rings.

Martin, the DEA administrator, said that actions against prescribers are not undertaken arbitrarily.
“When we are investigating something like a doctor that may be overprescribing, you know because we're not doctors, in the course of our investigation we are going to solicit medical experts,” Martin said. “We'll try to get what's called prescription drug monitoring program information and that's information that the states have at their level that shows how many prescriptions are being written by a doctor for a patient and being filled at a certain pharmacy."
“So we'll try to look at that stuff and then maybe go out to that pharmacy and do an inspection and look at their records and just see if there's anything more there and then we'll follow up with that,” he said.
Roughly 800 prescribers each year surrender their DEA registration – a kind of license – when the agency opens an investigation. DEA investigations can involve having assets and medical records seized. In some cases that can lead to bankruptcy, doctors said, prompting many to surrender their opioid prescribing rights, rather than fight a battle against a behemoth government.
Ibsen was an emergency room doctor in Montana when he became - as he puts it, an “accidental pain doctor,” taking “pain refugees” whose doctors had been arrested. Many patients were very ill and suffered severe chronic pain, said Ibsen, who added he was able to wean many patients down to lower doses.
Ibsen said he became a target of the state board of medical examiners after an employee he fired filed a complaint, saying he over-prescribed. His license was suspended but eventually reinstated – after four years. But he decided to stop prescribing opioids after five visits from the DEA.
“They were very vague,” he said of the DEA agents. “They said ‘You’re risking your freedom by prescribing to patients like these.’ I said ‘Patients like what?’ They said, ‘Patients who might sell the pills.’”
“Doctors are taking plea deals because they don’t want to go to prison,” said Ibsen, who was not charged. “Once they arrest a doctor, they seize all their medical records. A doctor can’t make any more income. They seize your assets, and can’t afford an attorney.”
Ibsen referred patients to a prominent pain doctor in California, Dr. Forrest Tennant, who became known for taking people cut off by other doctors. Tennant for years had been researching non-opioid alternatives.
Then the DEA raided Tennant’s office. The agency never charged him, but he, too, gave up prescribing opioids.
“It’s immoral and unsafe to forcibly taper down or abandon a patient,” said Tennant, whose patients included those with terminal illnesses. “Some doctors don’t give these patients any withdrawal medication. Who is the worst offender, then? The CDC, the DEA, the U.S. attorneys who are shutting down doctors, or the doctors who abandon patients?”
One Tennant patient, Jennifer Adams, a former Montana police officer who had been treated by Ibsen, died from a self-inflicted gunshot in April, after the California doctor’s office was raided by the DEA.
Tennant said he respects the idea “the DEA has a right and responsibility to investigate.”
“But since I used high doses, they said my patients were going to overdose and die,” Tennant said. “I’ve been practicing a long time, I’ve not had a single overdose. I’ve given patients thousands of opioid equivalents. I know how patients should be monitored.”
Dr. Lesly Pompy was one of a few pain physicians in a rural part of Michigan, serving as many as 1,500, the majority of them referrals from other doctors who could not treat their chronic conditions. A pain specialist since 1995, he kept long hours, sometimes going to hospital emergency rooms when he was summoned to help a patient in severe pain. Sometimes he would try nerve blocks, many other times opioids.
On Sept. 26, 2016, roughly 25 law enforcement officers raised Pompy’s office at the ProMedica Monroe Regional Hospital.
“There were DEA agents, county and local police, they had everybody in my waiting room and who worked in my office put their hands up. Children were crying. There was a helicopter over the building. It was like a scene from a Jason Bourne movie," he said.
Pompy was charged with unlawful distribution of prescription drugs and health care fraud from 2012 to 2016. A federal jury indicted him this summer on 37 counts. The indictment maintained Pompy illegally prescribed some 10 million dosage units of controlled substances that fell outside the realm of standard practice. He was also accused of inappropriately filing claims to insurers.
Pompy denies the charges and claims that because he prescribed large quantities of opioids, some to severe pain patients who require high doses, he became a target.
"The damage that the proliferation of opioid distribution has done to our community, like many across the United States has been devastating,” U.S. Attorney Matthew Schneider said, according to published reports. “It’s particularly disturbing when the distributor is a medical professional.”
Pompy’s former patients and some former employees have stood by him, saying he is being scapegoated. Former patients have held rallies and started a Facebook group in support of him.
Janet Zureki, a former patient of Pompy, said that -- as often happens after a prescriber's arrest -- patients were left in limbo, having to scramble to find another pain doctor. “After the raid and he could no longer prescribe, everyone was dangerously cut off of their medicines, including me,” she said. “It took me three months to find another pain doctor and they put me on a lower dose of medicine. During that three month period, I had to go without medicine and go through withdrawal.”
Zureki defends Pompy.
“As a doctor, I found him to be very compassionate and he also ran a tight ship,” she said. “I have been in his office and have heard him address someone who wasn’t taking their medicine properly, so I know he didn’t stand for that. He worked tirelessly to help the people in our community,” she said.
DOCTORS LAMENT WALKING AWAY
Nadeau is bewildered over having to stop treating his pain patients, at least one of whom died by suicide. And he said his hospital’s decision to stop working with opioids is by no means unique.
Hospitals increasingly see opioids as a liability; an overdose can land them in a lawsuit, he said. But he wrestles with the fact there are people he can no longer help.
“I can’t provide comprehensive care for my patients, meaning treatment of pain, depression, sleep problems, anxiety, and other problems,” Nadeau said. “In patients with chronic pain, there nearly always are a lot of problems.”
Nadeau reached out to fellow physicians to see if they would take his pain patients.
“It’s been extremely difficult to find physicians to provide comprehensive pain therapy,” he said. “I don’t blame physicians for being scared to death and for prescribing to CDC guidelines, but I do blame [some of] them for treating patients badly.”
For his part, Ibsen is treating patients with medical marijuana. Ibsen said he always strived to get patients on opioids to agree to taper down, and about 80 percent did, often using medical cannabis. For the others, opioids were the best treatment, Ibsen said. He understands the threat of the overdose epidemic all too well.
“My nephew died of a heroin overdose” in the summer, he said. “But incarcerating doctors is not going to solve the addiction crisis.”
“There are two things doctors do – we save lives and we relieve suffering. If we’re not willing now to relieve suffering, then what are we about?”









































