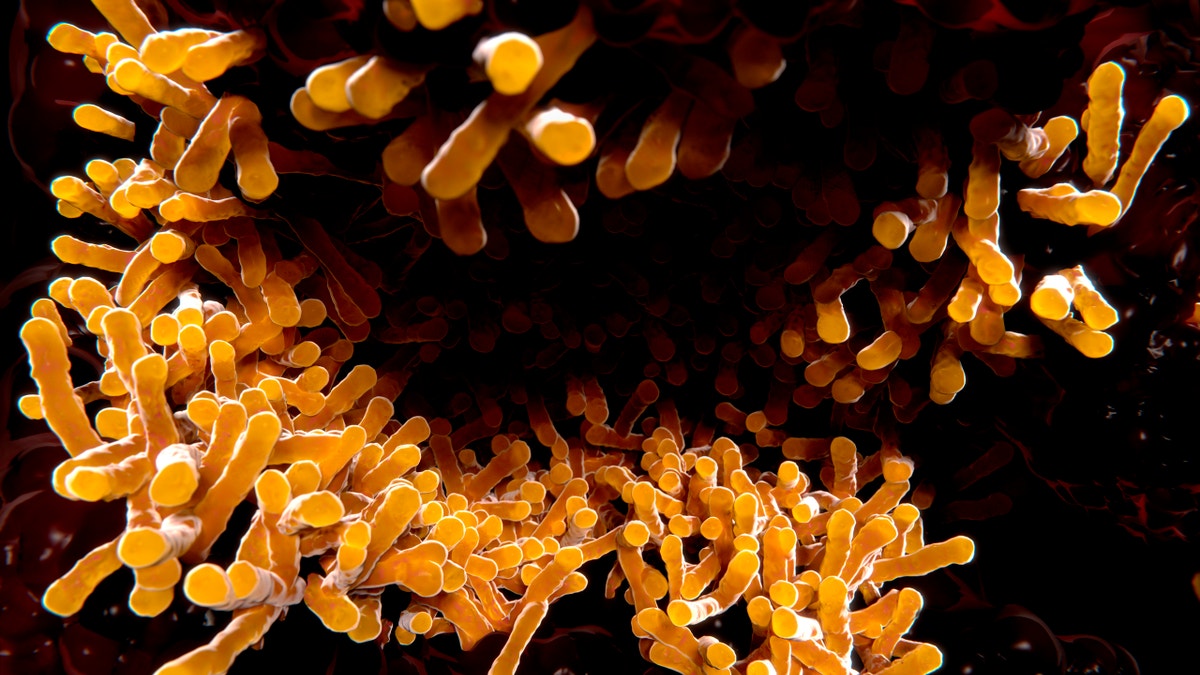
An image of tuberculosis bacillus. (iStock)
The next time your doctor prescribes— or refuses to prescribe— antibiotics for an illness, you might want to listen and follow directions exactly.
Misuse of antibiotics is a big contributor to the growing threat of so-called superbugs, bacterial infections that are difficult or impossible to treat. According to the Centers for Disease Control and Prevention, 2 million people develop such infections in the United States every year, resulting in about 23,000 deaths and more than $20 billion in excess health care costs.
READ MORE: All About Drug Formularies and Prescription Coverage
Taking antibiotics when you don’t need the, and failing to take a full course of antibiotics when you do each contribute to the growing risk of a superbug epidemic.
Here’s more about that risk, and how you can help stave it off:
How superbugs are made
In the centuries before penicillin was discovered, people frequently died young of bacterial infections that spiraled out of control. Usually, the source of the infection was something we now consider unthreatening— a bladder infection, or a cut on your finger while cooking dinner.
Since the advent of antibiotics, they’ve become such common, cheap prescriptions that most people no longer see them as lifesaving medicine. In a recent survey of 400 people by the American Society for Microbiology, 25 percent of respondents said they would use antibiotics without a prescription and 14 percent were keeping old antibiotics at home for future use.
About 5 percent of those surveyed said they had used antibiotics in the past year without a prescription, most often to treat ailments such as coughs, sinus infections and sore throats— symptoms that aren’t improved by antibiotics.
When bacteria are exposed to antibiotics, but not enough to kill the entire colony, only the strongest are left. Those remaining bacteria divide and continue to replicate, making the post-antibiotic colony stronger than the original and resistant to the antibiotic.
However, the issue is a lot more complicated than that, says Dr. Robin Patel, director of the Infectious Diseases Research Laboratory at the Mayo Clinic in Rochester, Minnesota.
READ MORE: What Preventive Care Is Free?
The sheer number of bacteria strains that exist make the issue complex. “We’re talking about a lot of different kinds of bacteria and a lot of different types of antibiotics at the same time,” Patel says.
The gene for antibiotic resistance is also easily spread from one bacterium to another when they come into contact, even if they are different species. In bacteria-rich environments, such as an animal or human intestine, this makes it possible for resistance to spread to several strains or species at once.
Because of this, taking antibiotics when you don’t need them may create resistant beneficial strains in your own body that can pass on resistance to less beneficial strains. As the bacteria adapt and become resistant faster than new antibiotics are being developed, more resistant strains are expected to appear.
Why the threat of antibiotic resistance is real
“Most people will not be affected by this in [the] next few years, but the trend is very frightening,” says Dr. Eric N. Milefchik, chairman of infection prevention at Torrance Memorial Medical Center in California. “Already, some healthy patients developing bladder infections in recent years have bacteria that can only be treated with intravenous antibiotics.”
READ MORE: How to Read Your Hospital Bill
The antibiotics that must be used for such infections, in general, “were developed over 20 years ago for the most resistant bacteria of the day,” Milefchik says. “The increased use of these antibiotics has given rise to the most feared superbugs to date.”
How you can help stop superbugs
On the surface, it seems like the obvious solution is just to develop more antibiotics. But because today’s antibiotics don’t turn much profit, there are few incentives for pharmaceutical companies to invest in the research and development to create new options.
READ MORE: The Real Difference Between Brand-Name and Generic Drugs
Still, we can all do our part to use antibiotics wisely, including not taking them when you don’t need to. “If you don’t need an antibiotic, there are definite downsides to taking one,” Patel says, including possible side effects that come with any medication.
Worse, Patel says antibiotics may also disrupt the beneficial bacteria in your body, together known as your microbiome, that help regulate your immune system and metabolism, among other things.
When it comes to antibiotics, make sure you and your family members follow these rules:
● Do take all doses of antibiotics you are prescribed, even if you feel better before they’re gone.
● Don’t pressure a doctor for antibiotics if he or she says you don’t need them. Many illnesses are viral, and antibiotics won’t fix your runny nose or common cold.
● Do throw away any old, unused antibiotics that are sitting in your medicine cabinet right now.
● Don’t take veterinary antibiotics or prescription drugs from outside the U.S., which may be compromised or ineffective.








































