Fox News Flash top headlines for September 14
Fox News Flash top headlines are here. Check out what's clicking on Foxnews.com.
Boosting a specific protein in the brain could help slow the progression of Alzheimer’s disease, a new study has found.
The longstanding theory is that Alzheimer’s occurs when a protein called amyloid-beta 42 (Aβ42) transforms into plaques that build up in the brain, causing damage to neural cells and leading to cognitive decline.
Researchers from the University of Cincinnati have challenged that assumption, instead suggesting that the disease is caused by low levels of healthy, functioning Aβ42, according to a UC press release.
They based this hypothesis on the fact that newly approved monoclonal antibody medications — including lecanemab (Leqembi) and donanemab (Kisunla) — have had the unintended outcome of raising levels of the protein in the brain.

Boosting a specific protein in the brain could help slow the progression of Alzheimer’s disease, a new study has found. (iStock)
"The new Alzheimer's treatments, which were designed to remove amyloid plaques, unintentionally raised Aβ42 levels, and this may explain their positive effects on cognition as much as — or better than — amyloid reduction," lead study author Alberto J. Espay, MD, professor of neurology at the Gardner Family Center for Parkinson's disease and Movement Disorders at UC, told Fox News Digital via email.
"Higher Aβ42 levels after treatment were associated with slower cognitive decline, suggesting that restoring this protein to normal levels might be more beneficial for Alzheimer’s patients than removing amyloid."
DEMENTIA WARNING: DON'T EVER SAY THESE 16 THINGS TO LOVED ONES WITH THE DISEASE, EXPERTS ADVISE
In the study, the researchers reviewed data from nearly 26,000 Alzheimer's patients who participated in 24 randomized clinical trials for the newly approved antibody treatments.
They compared the cognitive abilities of patients before and after taking the new medications, and found that the increased amounts of Aβ42 were linked to "slower cognitive impairment and clinical decline."
The findings were published in the medical journal Brain on Sept. 11.
Understanding amyloid
Amyloid plaques aren’t necessarily a bad thing, according to the researchers.
"Along with other studies, the collective evidence suggests that amyloid plaques are a response of a normally reactive brain to many stressors, some infectious, some toxic, some biological," Espay told Fox News Digital.
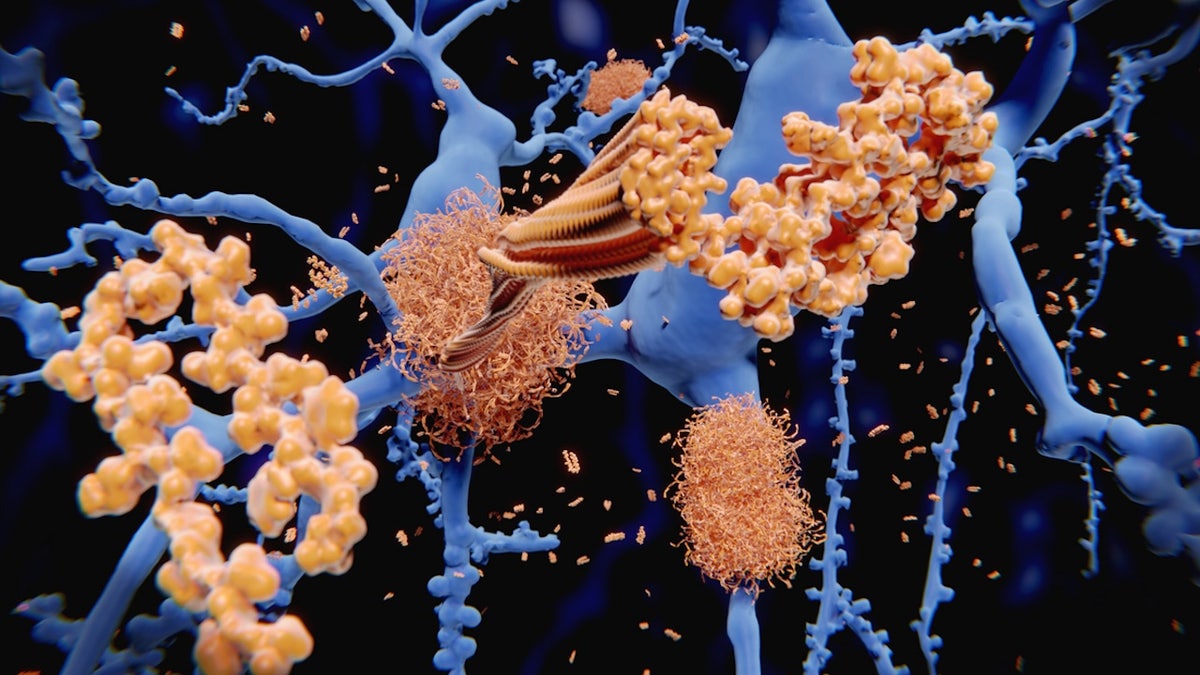
The longstanding theory is that Alzheimer’s occurs when a protein called amyloid-beta 42 (Aβ42) transforms into plaques that build up in the brain, causing damage to neural cells and leading to cognitive decline. (iStock)
"They are a sign the brain is dealing with a stressor appropriately."
The researcher referred to amyloid plaques as "the tombstones of Aβ42," noting that they can’t do anything harmful to the brain.
"Most researchers do not believe Alzheimer’s is driven by only one biological mechanism."
"Amyloid plaques don’t cause Alzheimer’s, but if the brain makes too much of them while defending against infections, toxins or biological changes, it can’t produce enough Aβ42, causing its levels to drop below a critical threshold," he said.
"That’s when dementia symptoms emerge."
The study questions the long-entrenched idea that amyloid plaques directly cause Alzheimer’s and that removing them is part of the solution.
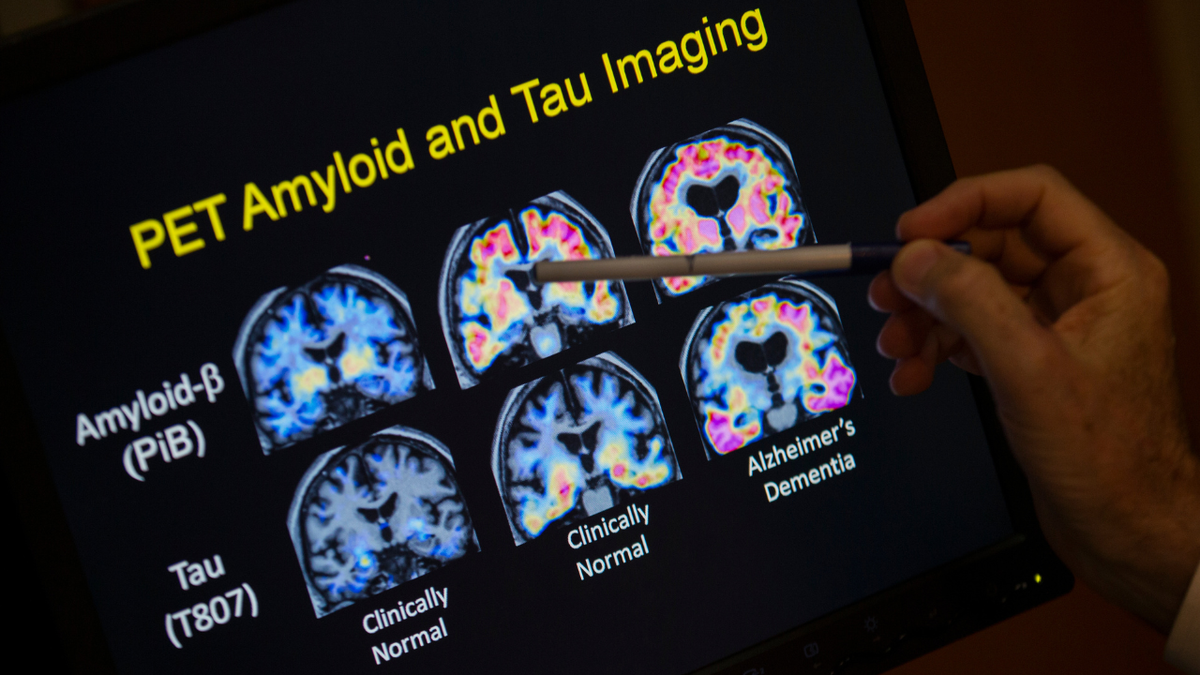
"Beta amyloid is certainly an important and key player, but we also know that tau protein, the immune system, vascular system, metabolic health, environment and more all play a role in the disease process," an Alzheimer's expert said. (AP Photo/Evan Vucci, File)
"Building the levels of Aβ42 without removing amyloid — which is quite futile, and can be harmful — is worth testing as a future therapy," Espay added.
Looking ahead, the UC research team plans to investigate therapies that directly increase Aβ42 levels without targeting amyloid.
‘A very complex disease’
Ozama Ismail, PhD, director of scientific programs at the Alzheimer’s Association in Chicago, was not involved in UC’s study, but commented on the findings.
CLICK HERE TO GET THE FOX NEWS APP
"While this Aβ42-related hypothesis may turn out to be a part of what causes and encourages progression of Alzheimer’s, it is a very complex disease, and most researchers do not believe Alzheimer’s is driven by only one biological mechanism," he told Fox News Digital.
DEMENTIA HAS 2 SHOCKING NEW RISK FACTORS, STUDY FINDS, WITH TOTAL OF 14 NOW ON LIST
"Beta amyloid is certainly an important and key player, but we also know that tau protein, the immune system, vascular system, metabolic health, environment and more all play a role in the disease process."
While FDA-approved drugs targeting amyloid are now available and in use, Ismail calls for a comprehensive approach to Alzheimer’s treatment that involves multiple approaches.

"Understanding the entire underlying biology and related mechanisms is important to expand our pipeline of treatments and prevention strategies," an expert said of Alzheimer's treatment. (iStock)
He recommends "a combination of therapies targeting multiple mechanisms, as well as lifestyle interventions, much like how other major diseases like diabetes, HIV/AIDS and heart disease are treated."
Added Ismail, "Understanding the entire underlying biology and related mechanisms is important to expand our pipeline of treatments and prevention strategies."
Potential limitations
Espay also acknowledged the limitation that none of the published studies have allowed access to the individual-level data.
For more Health articles, visit www.foxnews.com/health
"We can only work with the group-level data published," he told Fox News Digital. "Despite this limitation, the results were robustly supported."
CLICK HERE TO SIGN UP FOR OUR HEALTH NEWSLETTER
Fox News Digital reached out to Biogen and Eisai (makers of Leqembi) and Eli Lilly (maker of Kisunla) requesting comment.











































