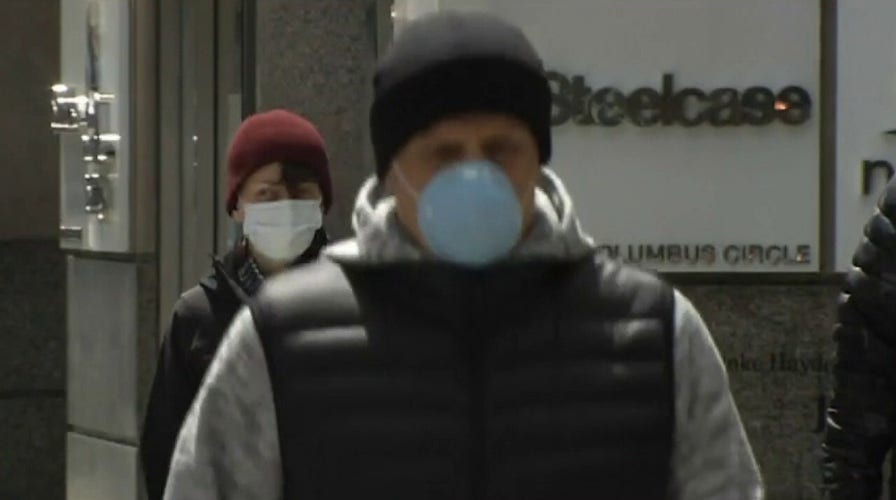
Dr. Siegel: 'Consistent compliance' needed to stop spread of COVID-19
Dr. Marc Siegel explains what America needs to do better as the U.S. surpasses 19 million coronavirus cases.
After reports surfaced of a "mysterious, pneumonia-like" illness in early 2020, the science and medical community undertook efforts to develop, manufacture and overcome regulatory hurdles for vaccines and treatments to combat the deadly novel coronavirus, hopefully finding a way out of the global pandemic at unprecedented speed.
Pfizer/BioNTech and Moderna are currently at the forefront of vaccines for COVID-19 disease caused by the SARS-CoV-2 virus, with both winning recent emergency approval from the U.S. Food and Drug Administration, and a nod from some international agencies. This has sparked the first stages of a historic mass immunization effort against a virus that has claimed over 1.7 million lives worldwide.
VACCINATED AGAINST COVID-19? STILL WEAR A MASK, SOCIAL DISTANCE, AZAR SAYS
Both of those vaccines involve a two-dose regimen administered about three weeks apart and they operate on a new platform with messenger RNA, or mRNA, technology. Pfizer's requires strict, sub-freezing storage conditions, but Moderna's is more distribution-friendly, with a 30-day shelf-life at normal refrigerator temperatures.
Nevertheless, health leaders are pushing for as many vaccine candidates as possible in order to meet global demand. In that regard, Johnson & Johnson is also working its way through the pipeline with a single-dose coronavirus vaccine, and a two-dose shot in a second trial. And there is another vaccine candidate developed by AstraZeneca and the University of Oxford, but that trial was paused temporarily because a participant in the study developed a severe but unspecified illness. In all, the World Health Organization lists 172 vaccines in early stages of development, and over 60 candidates under testing.
However, regulatory approvals for vaccines surfaced only in the last month of 2020, and at-risk health care workers manning the front lines for the past 10 months have also been driven in their search to treat patients already with the disease. Early reports suggested turning patients onto their stomach in a bid for a greater chance at recovery, while others suggested infusing coronavirus-ill patients with convalescent plasma containing recovered patients’ antibodies, in the hopes of a boosted immune response.
LIVE UPDATES: TODAY'S LATEST COVID-19 HEADLINES
In August, President Trump gave emergency authorization for convalescent plasma to treat coronavirus patients. He called it a "major breakthrough."
As the country eagerly awaited coronavirus vaccines, and some semblance of normalcy, pharmaceutical giant Eli Lilly received FDA emergency approval for an investigational monoclonal antibody treatment. The FDA also gave Regeneron Pharmaceuticals' COVID-19 antibody therapy, an experimental treatment that President Trump said helped cure him of the disease, emergency approval.
Monoclonal antibodies are best used early in the course of the disease. Ideally, the treatment should be given promptly after a positive diagnosis to help prevent high-risk people from progressing into more severe stages of the illness. In recent weeks, Health and Human Services Secretary Alex Azar has repeatedly advised coronavirus-positive individuals over 65 and those under 65, but considered higher risk, to promptly ask health care workers about Regeneron or Eli Lilly’s monoclonal antibody treatments.
Gilead Sciences antiviral drug remdesivir also cleared regulatory hurdles in a bid for improved recovery among hospitalized patients. Azar lauded promising results from a National Institutes of Health clinical trial, and in late fall, a second authorization for remdesivir, this time in combination with rheumatoid arthritis drug baricitinib, was authorized to treat hospitalized patients 2 years or older who need supplemental oxygen. Not all touted remdesivir in the treatment against coronavirus, however; the World Health Organization rejected the drug after it was shown to have "little or no effect" during the agency’s multicountry Solidarity Trial.
Nevertheless, the testing of therapeutics, including malaria treatment hydroxychloroquine, which proved useless in a WHO trial, is part of the process, health leaders have said because safety takes top priority in vaccine trials.
Ultimately, while federal officials with Operation Warp Speed, the mission to develop and distribute a COVID-19 vaccine, and Dr. Anthony Fauci, the nation’s leading infectious disease expert, had lauded scientific advancements for the fast development and approval process, vaccines will serve no use if the public is unwilling to take them.
In December, which was deemed the worst month for COVID-19 to date with at least 5.3 million reported cases, Fauci said community engagement and outreach were essential to overcome distrust in vaccines.
"We’ve got to be doing a lot of community engagement and community outreach to get people to understand the two things that bother people, they say, ‘Well, maybe we did this too quickly,’" Fauci said during the virtual Bloomberg American Health Summit 2020. "They need to understand the speed is really a reflection of the extraordinary scientific advances that have been made that allowed us to do things in weeks to months that normally would’ve taken several years."
U.S. officials will likely fall short of an original goal to vaccinate 20 million Americans by the end of 2020. But officials anticipate millions of additional doses will be distributed next year, and they continue to plead with the public to follow mitigation measures like wearing masks, avoiding crowds, keeping a proper distance from others and washing hands. These measures should continue even after vaccinations, while researchers work to understand what effect of the recently approved vaccines have on virus spread.