Coronavirus outbreak: How to help your mental health
Psychotherapist Dr. Kathryn Smerling gives tips on handling mental health during coronavirus, including rewarding yourself and staying organized.
Get all the latest news on coronavirus and more delivered daily to your inbox. Sign up here.
As the coronavirus continues to tear through the United States, front-line health-care workers are not only in the line of fire, but they are also caught amid growing concern that medical facilities themselves could become hubs for transmission.
What's more, global experts worry that the U.S. will soon take the baton from China and Italy, becoming the epicenter for the disease's spread.
"Health-care workers are living in a state of constant anxiety and fear — fear of exposure from sick patients, of getting sick themselves, of accidentally bringing the virus home to loved ones," Dr. Summer McGee, dean of the School of Health Sciences at the University of New Haven, told Fox News. "Every day is filled with compromises, tradeoffs, and life-and-death decisions on a scale and regularity that our health-care system has never seen."

A U.S. health care worker wearing a homemade mask for protection while working (Provided to Fox News)
Through her lens, one of the biggest concerns now is that health-care professionals "know they are working in suboptimal and, in some cases, outright unsafe working conditions."
"Many hospitals are telling workers that you cannot even use masks or other personal protective equipment (PPE) until they have confirmed that a patient has COVID-19, but tests aren't available for COVID-19. These health-care workers are playing Russian roulette with every patient they treat," she stressed. "Having to ration, reuse, or entirely go without proper protective equipment is a major concern. Many health-care organizations have PPE today but only have a two-week supply."
WHY JAPAN APPEARS TO HAVE AVOIDED A MASS CORONAVIRUS OUTBREAK
In recent weeks, the novel pathogen – which is believed to have originated in a Chinese wet market late last year – has infected more than 64,500 Americans and killed over 900. As of Wednesday afternoon, more than 12 states have reported more than 1,000 cases, with New York registering over 26,400, followed by neighboring New Jersey at 3,675 and California at almost 2,700.

The newly renamed Hotel 166, located near the Northwestern University Hospital complex, in a Monday photo. (AP Photo/Charles Rex Arbogast)
The United States represents 13.5 percent of the world's confirmed cases and some 4.2 percent of its fatalities – a figure that is climbing by the hour. Subsequently, the supply of vital PPE has seemingly not been able to keep up with the escalating demand, given the fast-acting nature of coronavirus, referred to officially as COVID-19.
Lawmakers and leaders also worry that a disproportionate infection rate among providers, rendering them ill and unable to work, will have the spiral effect of deepening the already existing calamity.
"Hospitals are already short-staffed as we are in a severe flu season. Long hours, shortage of protective gear, and testing limitation have some fearing that they are flying blind," explained Dr. Azadeh Shirazi, a board-certified surgeon, disease specialist and founder of the California-based La Jolla Laser Surgery Center. "It's a harrowing scene when you are not protecting a limited supply of trained workers. We cannot afford to lose them."
Beyond just the doctors and nurses in medical facilities, overrun and ill-outfitted hospitals as transmission points also threaten other vital services, including security and cleaning personnel. Moreover, the disease has ravished police and firefighting departments nationwide, and scores of EMTs are also grappling with high numbers of diagnoses among the ranks.
Fox News interviewed a number of frontline medical workers across the country, who could only speak on the condition of anonymity because they were under strict mandates not to talk to the press about the developing situation.

New York-Presbyterian says visitors will no longer be allowed inside the labor and delivery units during the coronavirus outbreak. (Google Maps)
One Mississippi-based emergency room physician noted that some staff this week have been put on leave after exhibiting symptoms linked to coronavirus, said that in one incidence, five patients from the same family all went into a critical condition – requiring ventilators – after being in close contact with another at a funeral a week prior to becoming ill.
"The public can help us by not exposing themselves or others and practicing social distancing," the doctor stressed.
The source depicted the emergency room scene in the state as akin to a "marathon," with the number of those requiring ventilators more than half of the confirmed cases, and staff working extended shifts for more than three weeks straight.
Dr. Dan Field, chief medical officer at MDstaffers, pointed out that with such demanding hours, many personnel are struggling to obtain safe and adequate child care.
"The best thing everybody can do to help the medical profession as follow the rules set down to flatten the curve by minimizing contact and risk of infection. Only go to the emergency department if you are sicker than a dog and feel like you are heading towards death," he said. "Otherwise, find some way of triaging yourself through telemedicine and similar no-contact communication."
Another New York doctor at a large hospital tending to a number of coronavirus patients early last week lamented that they had fast run out of PPE, and had resorted to reusing n95 masks and even brown paper masks. In another New York hospital, a diagnostic sonographer expressed frustration at a mandate not to wear masks because patients had complained that it gave them anxiety, igniting an extra layer of stress for the workers and their families.
Furthermore, many experts fear that – given China's initial smothering of information related to the virus and the incorrect information about its transmission stemming from the World Health Organization (WHO) in the first few critical weeks of the outbreak – the deadly pathogen was swarming unchecked through hospitals and doctor's offices for weeks.
While at least 15 states have issued stay-at-home orders and shuttered nonessential businesses, local governments in many other pockets of the country are now being forced to adopt similarly stringent measures including closing public places and restaurants, as well as prohibiting medical procedures and surgeries considered not to be immediately required to ensure as much space and resources in left amid the coronavirus battle.
"We just lost a young nurse in Saint Louis to the Wuhan virus," lamented Dr. Scott Magill, executive director of Veterans in Defense of Liberty and former U.S. Army Medical Corps soldier. "Watching these medical warriors, doctors, nurses and hospital staff, placing themselves and their families in grave danger for the sake of humanity, is emotionally powerful."
And Dr. Josh Luke, a Los Angeles-based hospital CEO – most recently Memorial Hospital of Gardena in Los Angeles County – opined that L.A. county officials and Orange County officials in California have been refusing his help, and has essentially been told, "We are not set up to bring on individuals. We are relying on the health systems to help with pop-up hospitals and overflow isolation hotels."
As a former hospital CEO and licensed nursing home administrator with significant experience managing ventilator units, Luke noted, the red tape is a restriction at a time of desperate need. He pointed out that doctors are being asked to come out of retirement to help, but the process of streamlining management is "clearly flawed."
After being turned away by L.A. county officials, Luke said he drove this week to a hotel in Pomona that's being converted to accommodate isolation overflow and was turned away by security.
WILL' HERD IMMUNITY' WORK AGAINST CORONAVIRUS?
Nonetheless, national data with regards to just how hard health-care personnel have been hit by coronavirus is not yet available from the Centers for Disease Control and Prevention (CDC).
Dr. Attila Hertelendy, a Florida-based expert in biomedicine and emergency and disaster management, also underscored that the usual burden already placed on the medical infrastructure has not suddenly dispersed due to the coronavirus onslaught, either.
"Most of the current challenges in our health-care facilities stem from managing the day to day patients that come to our facilities, these patients that have chronic conditions requiring daily treatment such as dialysis, chemotherapy, etc. They don't go away just because there is a coronavirus pandemic," he said. "Finding ways to continue to provide high-quality care for vulnerable patient groups such as the disabled, elderly remains a challenge as resources are diverted to manage an escalating number of cases daily."
Despite broad criticism over a lack of preparedness for such a public health crisis, a late 2019 assessment by the Nuclear Threat Initiative (NTI) and the Johns Hopkins Center for Health Security (JHCHS) ranked the United States as the best-prepared country in the world to handle a pandemic.
President Trump this week acknowledged that the pandemic is likely to worsen but has assured workers that federal authorities are addressing concerns surrounding specialized masks and surgical gowns, with shipments on their way. On Wednesday, Trump affirmed that FEMA was distributing 8 million medical masks and 14 million surgical masks.
CLICK HERE FOR FULL CORONAVIRUS COVERAGE
U.S. officials have reached out to South Korea for assistance in obtaining the needed supplies to fight the pandemic, as tensions ramp up between Washington and Beijing – which has typically outsourced much of the world with such medical needs – over the virus. The unrest swirls amid veiled threats from the Communist leadership that supplies would be withheld should they be saddled with coronavirus blame.
Moreover, the sudden onslaught of the coronavirus has also illuminated the ingenuity and selflessness of the many American individuals and private companies. According to New York Gov. Andrew Cuomo, more than 40,000 health-care professionals have signed on as volunteers to offer assistance in New York alone – some 6,000 of them in the realm of mental health care to provide free online services to those in need.
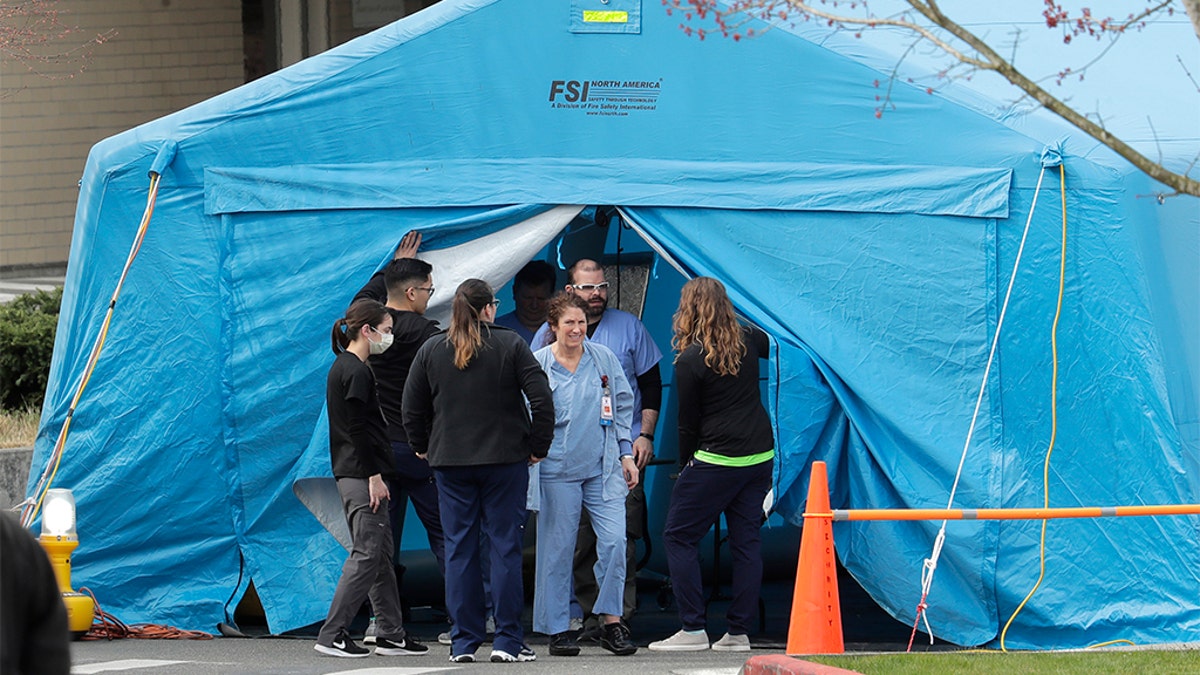
A large tent set up in front of the emergency room at EvergreenHealth Medical Center in Kirkland, Wash., last week. (AP Photo/Ted S. Warren)
Other non-traditional businesses – from car and electronic manufacturers to small apparel companies – have also taken to making such crucial medical supplies, including respirators, ventilators, masks, and gowns. Companies developing at-home testing kits have over the past week even reversed course and opted to send their technologies instead to medical facilities as the first priority.
CLICK HERE FOR THE FOX NEWS APP
However, others are more skeptical regarding what lies ahead as the caseload across the country swells.
"Once our ventilator and ICU capacity has run out, doctors and administrators must be prepared for how they will make rationing decisions, on the ground and in real-time, of who will get lifesaving care and who will not," McGee added. "Everyone is talking about ICU bed and ventilator capacity, but I am worried about healthcare worker and staffing capacity. Once healthcare workers begin to get who can step in to provide care? I do not see that we have a solid plan for that."

